Shingles treatment involves antiviral medications and pain relief strategies to manage symptoms effectively. At HOW.EDU.VN, our team of experienced doctors provides personalized treatment plans to alleviate your discomfort and prevent complications, offering guidance on managing the rash and associated nerve pain. Connect with our experts to explore advanced therapies, discover effective home remedies, and get comprehensive support for post-herpetic neuralgia.
1. What is Shingles and Why Does It Occur?
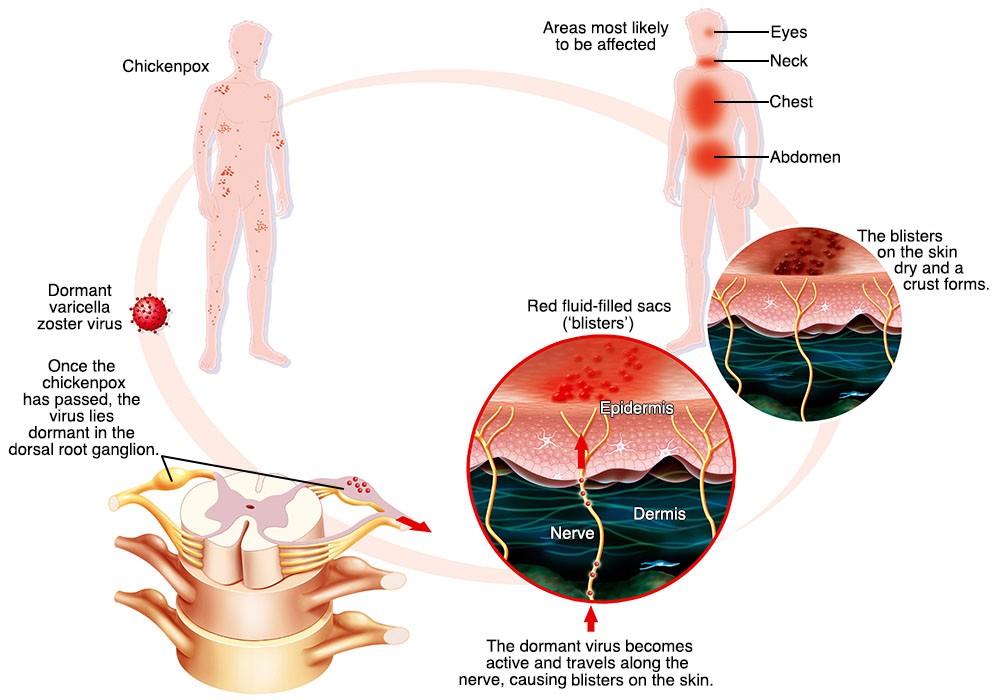
Shingles, also known as herpes zoster, is a viral infection that causes a painful rash. The varicella-zoster virus (VZV), the same virus that causes chickenpox, is responsible for this condition. After a person recovers from chickenpox, the virus remains dormant in nerve tissues. Shingles occurs when the virus reactivates later in life.
Several factors can trigger the reactivation of the virus, including:
- Weakened Immune System: Conditions or treatments that suppress the immune system, such as HIV/AIDS, cancer, or immunosuppressant drugs, can increase the risk.
- Age: The risk of shingles increases with age, particularly after 50, due to the natural decline in immune function.
- Stress: High levels of physical or emotional stress can weaken the immune system, potentially leading to viral reactivation.
- Certain Medical Conditions: Chronic illnesses like diabetes and heart disease can compromise immune function, making individuals more susceptible.
- Medications: Some medications, such as corticosteroids, can suppress the immune system and increase the risk of shingles.
According to a study by the Centers for Disease Control and Prevention (CDC), about 1 in 3 people in the United States will develop shingles in their lifetime. If you’re experiencing any of these risk factors or suspect you have shingles, connect with our experts at HOW.EDU.VN for a comprehensive consultation and personalized treatment plan.
2. What Are the Early Signs and Symptoms of Shingles?
Recognizing the early signs and symptoms of shingles is crucial for prompt treatment and minimizing complications. The initial symptoms often precede the appearance of the rash and may include:
- Pain, Burning, or Tingling: These sensations typically occur on one side of the body and can range from mild to severe.
- Numbness or Itching: The affected area may feel numb or intensely itchy.
- Sensitivity to Touch: The skin may become unusually sensitive to touch, even light pressure.
- Headache: Some individuals experience headaches as an early symptom.
- Fatigue: Feeling unusually tired or fatigued is another common early sign.
- Fever: A low-grade fever may accompany the other initial symptoms.
How to Recognize the Shingles Rash
The hallmark of shingles is a painful rash that develops in a specific pattern. The rash typically appears as:
- Location: Usually on one side of the body, often in a band-like pattern following a nerve pathway (dermatome).
- Appearance: Starts as red bumps that turn into fluid-filled blisters.
- Progression: Blisters may break open, ooze, and eventually crust over.
- Duration: The rash typically lasts for 2 to 4 weeks.
Seeking Early Medical Attention
If you experience any of these symptoms, especially if you have a history of chickenpox, it’s essential to seek medical attention immediately. Early treatment with antiviral medications can significantly reduce the severity and duration of the illness.
At HOW.EDU.VN, our team of doctors can provide a prompt diagnosis and initiate an effective treatment plan to manage your symptoms and prevent complications. Contact us today for expert care and guidance.
3. How is Shingles Diagnosed by a Healthcare Professional?
Diagnosing shingles typically involves a thorough medical history review and a physical examination. During the consultation, a healthcare professional will:
- Review Your Medical History: This includes asking about previous chickenpox infections, vaccinations, and any underlying health conditions that may weaken your immune system.
- Assess Your Symptoms: The doctor will inquire about the specific symptoms you’re experiencing, such as pain, tingling, itching, and the location and nature of the rash.
- Conduct a Physical Examination: The doctor will examine the rash to determine if it matches the typical presentation of shingles. This includes looking at the distribution, appearance (red bumps, blisters, crusting), and any signs of secondary infection.
Diagnostic Tests
In most cases, the clinical presentation of shingles is sufficient for diagnosis. However, in certain situations, additional tests may be necessary to confirm the diagnosis or rule out other conditions. These tests include:
- Viral Culture: A sample of fluid from the blisters is collected and sent to a laboratory to identify the presence of the varicella-zoster virus (VZV).
- Polymerase Chain Reaction (PCR) Assay: This highly sensitive test detects VZV DNA in blister fluid or skin scrapings.
- Tzanck Smear: A quick test where cells from the base of a blister are examined under a microscope to look for characteristic viral changes.
- Blood Tests: Blood tests are generally not used to diagnose shingles but may be performed to assess overall immune function or rule out other conditions.
Ruling Out Other Conditions
It’s important to differentiate shingles from other conditions that can cause similar symptoms, such as:
- Herpes Simplex Virus (HSV) Infections: HSV can cause blisters, but they typically occur in different locations (e.g., mouth, genitals).
- Contact Dermatitis: An allergic reaction to substances like poison ivy can cause a rash, but it usually lacks the characteristic dermatomal distribution of shingles.
- Impetigo: A bacterial skin infection that can cause blisters and crusting, but it’s not associated with nerve pain.
At HOW.EDU.VN, our experienced doctors utilize a combination of clinical assessment and diagnostic testing to ensure an accurate diagnosis and appropriate treatment plan. If you suspect you have shingles, contact us for a comprehensive evaluation and personalized care.
4. What Are the Most Effective Medical Treatments for Shingles?
The primary goal of medical treatment for shingles is to reduce the severity and duration of the illness, as well as to prevent complications such as post-herpetic neuralgia (PHN). The most effective treatments include antiviral medications, pain management, and supportive care.
Antiviral Medications
Antiviral drugs are the cornerstone of shingles treatment. These medications work by inhibiting the replication of the varicella-zoster virus (VZV), thereby reducing the severity and duration of the infection. The most commonly prescribed antiviral medications for shingles include:
- Acyclovir (Zovirax): This is one of the oldest and most widely used antiviral drugs for shingles. It’s available in oral, topical, and intravenous formulations.
- Valacyclovir (Valtrex): A prodrug of acyclovir, valacyclovir is better absorbed by the body, allowing for less frequent dosing.
- Famciclovir (Famvir): Similar to valacyclovir, famciclovir is a prodrug that is converted into penciclovir, an active antiviral compound.
Key Considerations:
- Timing: Antiviral medications are most effective when started within 72 hours of the onset of the rash. Early treatment can significantly reduce the risk of complications.
- Dosage and Duration: The dosage and duration of antiviral treatment will depend on the specific medication, the severity of the infection, and the patient’s overall health.
- Side Effects: Common side effects of antiviral medications include nausea, vomiting, headache, and dizziness.
Pain Management
Pain is a significant symptom of shingles, and effective pain management is crucial for improving the patient’s quality of life. Pain management strategies include:
- Over-the-Counter Pain Relievers: Non-prescription pain relievers such as acetaminophen (Tylenol) and nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen (Advil, Motrin) can help alleviate mild to moderate pain.
- Prescription Pain Medications: For more severe pain, prescription pain medications such as opioids (e.g., codeine, oxycodone) may be necessary. However, these medications should be used with caution due to the risk of addiction and side effects.
- Topical Treatments: Topical creams and lotions containing capsaicin or lidocaine can provide localized pain relief.
- Nerve Pain Medications: Medications such as gabapentin (Neurontin) and pregabalin (Lyrica) are often prescribed to treat nerve pain associated with shingles and PHN.
- Corticosteroids: In some cases, corticosteroids such as prednisone may be used to reduce inflammation and pain. However, their use is controversial due to potential side effects.
Additional Medical Treatments
- Calamine Lotion: Applying calamine lotion to the rash can help relieve itching and discomfort.
- Cool Compresses: Applying cool, moist compresses to the affected area can help soothe the skin and reduce inflammation.
- Antihistamines: Oral antihistamines can help relieve itching.
- Antibiotics: If the rash becomes infected with bacteria, antibiotics may be necessary.
At HOW.EDU.VN, our team of doctors develops individualized treatment plans based on the patient’s specific needs and symptoms. We carefully consider the risks and benefits of each treatment option to ensure the best possible outcome. If you’re seeking expert medical care for shingles, contact us today to schedule a consultation. Address: 456 Expertise Plaza, Consult City, CA 90210, United States. Whatsapp: +1 (310) 555-1212.
5. Are There Effective Home Remedies to Alleviate Shingles Symptoms?
In addition to medical treatments, several home remedies can help alleviate the symptoms of shingles and promote healing. These remedies focus on reducing pain, soothing the skin, and supporting the immune system.
Natural Pain Relief
- Cool Compresses: Applying cool, moist compresses to the affected area can help reduce pain and inflammation. Soak a clean cloth in cool water, wring out the excess, and apply to the rash for 15-20 minutes several times a day.
- Colloidal Oatmeal Baths: Colloidal oatmeal has anti-inflammatory properties that can help soothe itchy, irritated skin. Add one cup of colloidal oatmeal to a lukewarm bath and soak for 15-20 minutes.
- Capsaicin Cream: Derived from chili peppers, capsaicin cream can help reduce nerve pain by desensitizing pain receptors. Apply a small amount to the affected area several times a day, but be cautious as it may cause a burning sensation initially.
- Honey: Honey has antibacterial and anti-inflammatory properties that can promote wound healing and reduce pain. Apply a thin layer of honey to the rash and cover with a clean bandage.
Skin Care
- Keep the Area Clean and Dry: Gently wash the affected area with mild soap and water, and pat dry. Avoid harsh scrubbing or abrasive cleansers.
- Calamine Lotion: Calamine lotion can help relieve itching and protect the skin. Apply a thin layer to the rash as needed.
- Avoid Scratching: Scratching the rash can increase the risk of secondary infection and scarring. Keep fingernails short and clean, and consider wearing gloves at night to prevent scratching while you sleep.
- Loose-Fitting Clothing: Wear loose-fitting, breathable clothing to avoid irritating the rash.
Diet and Supplements
- Boost Your Immune System: Consume a healthy diet rich in fruits, vegetables, and whole grains to support your immune system.
- Vitamin C: Vitamin C is an antioxidant that can help boost immune function. Consider taking a vitamin C supplement or eating foods high in vitamin C, such as citrus fruits and berries.
- Vitamin B12: Vitamin B12 is important for nerve health and may help reduce nerve pain. Good sources of vitamin B12 include meat, fish, eggs, and dairy products.
- Lysine: Lysine is an amino acid that may help inhibit the replication of the herpes zoster virus. Consider taking a lysine supplement or eating foods high in lysine, such as legumes, fish, and poultry.
Stress Management
- Stress Reduction Techniques: High levels of stress can weaken the immune system and exacerbate shingles symptoms. Practice stress reduction techniques such as yoga, meditation, or deep breathing exercises.
- Adequate Rest: Getting enough sleep is essential for immune function and healing. Aim for 7-9 hours of sleep per night.
While home remedies can provide relief from shingles symptoms, they should not replace medical treatment. If your symptoms are severe or if you develop complications, seek medical attention immediately. At HOW.EDU.VN, our team of doctors can provide comprehensive care and guidance to help you manage shingles effectively.
6. How Can Shingles Be Prevented Through Vaccination?
Vaccination is the most effective way to prevent shingles and its complications. The shingles vaccine is recommended for adults aged 50 years and older, regardless of whether they have had chickenpox. There are two shingles vaccines available in the United States:
- Shingrix (Recombinant Zoster Vaccine): Shingrix is the preferred shingles vaccine due to its high efficacy and long-lasting protection. It is a non-live vaccine, meaning it does not contain a weakened form of the virus. Shingrix is administered in two doses, given 2 to 6 months apart. Studies have shown that Shingrix is more than 90% effective in preventing shingles and PHN in adults aged 50 and older.
- Zostavax (Zoster Vaccine Live): Zostavax is a live, attenuated vaccine that was previously recommended for shingles prevention. However, it has been replaced by Shingrix due to its lower efficacy and shorter duration of protection. Zostavax is no longer available in the United States since November 2020.
Who Should Get the Shingles Vaccine?
- Adults Aged 50 Years and Older: The CDC recommends that all adults aged 50 years and older receive the Shingrix vaccine, even if they have had shingles before or are unsure if they have had chickenpox.
- Individuals Who Have Had Shingles: Even if you have had shingles in the past, you can still get the shingles vaccine to prevent future occurrences.
- Individuals Who Received Zostavax: If you previously received the Zostavax vaccine, you should still get the Shingrix vaccine for better protection.
Who Should Not Get the Shingles Vaccine?
- Individuals Who Are Allergic: People who have had a severe allergic reaction to any component of the vaccine should not receive it.
- Individuals Who Are Pregnant or Breastfeeding: Shingrix has not been studied in pregnant or breastfeeding women, so it is not recommended for these populations.
- Individuals with Weakened Immune Systems: While Shingrix is generally safe for people with weakened immune systems, it’s important to discuss your individual situation with your doctor.
Benefits of Vaccination
- High Efficacy: Shingrix is highly effective in preventing shingles and PHN.
- Long-Lasting Protection: Protection from Shingrix lasts for several years.
- Reduced Risk of Complications: Vaccination can reduce the risk of serious complications such as PHN, vision loss, and neurological problems.
Vaccination is a safe and effective way to protect yourself from shingles. At HOW.EDU.VN, our team of doctors can provide you with personalized advice on shingles vaccination and help you schedule your vaccine appointment. Contact us today to learn more.
7. What Are the Potential Complications of Shingles If Left Untreated?
If left untreated, shingles can lead to several complications, some of which can be severe and long-lasting. Early diagnosis and treatment are crucial to minimize the risk of these complications.
Post-Herpetic Neuralgia (PHN)
PHN is the most common complication of shingles, affecting up to 10-18% of individuals who develop the condition. PHN is characterized by chronic nerve pain that persists for months or even years after the shingles rash has healed. The pain can be severe and debilitating, interfering with sleep, work, and daily activities. Treatment for PHN may include:
- Topical Treatments: Creams and lotions containing capsaicin or lidocaine can provide localized pain relief.
- Nerve Pain Medications: Medications such as gabapentin (Neurontin) and pregabalin (Lyrica) are often prescribed to treat nerve pain.
- Tricyclic Antidepressants: Antidepressants such as amitriptyline and nortriptyline can also help relieve nerve pain.
- Opioids: In severe cases, opioids may be necessary, but they should be used with caution due to the risk of addiction.
Ophthalmic Shingles
Ophthalmic shingles occurs when the shingles virus affects the ophthalmic branch of the trigeminal nerve, which supplies sensation to the eye and surrounding structures. This can lead to serious eye complications, including:
- Conjunctivitis: Inflammation of the conjunctiva, the membrane that lines the eyelid and covers the white part of the eye.
- Keratitis: Inflammation of the cornea, the clear front part of the eye.
- Uveitis: Inflammation of the middle layer of the eye.
- Glaucoma: Increased pressure inside the eye, which can damage the optic nerve and lead to vision loss.
- Vision Loss: In severe cases, ophthalmic shingles can cause temporary or permanent vision loss.
Ramsay Hunt Syndrome
Ramsay Hunt syndrome occurs when the shingles virus affects the facial nerve near the ear. This can lead to:
- Facial Paralysis: Weakness or paralysis of the muscles on one side of the face.
- Hearing Loss: Damage to the auditory nerve can cause hearing loss.
- Vertigo: A sensation of spinning or dizziness.
- Rash Around the Ear: A painful rash with blisters may develop around the ear.
Bacterial Infections
The shingles rash can become infected with bacteria if the blisters are scratched or broken. Bacterial infections can lead to:
- Cellulitis: A deep skin infection that can cause redness, swelling, and pain.
- Impetigo: A superficial skin infection that causes blisters and crusting.
- Scarring: Severe bacterial infections can lead to permanent scarring.
Neurological Complications
In rare cases, shingles can lead to neurological complications such as:
- Encephalitis: Inflammation of the brain.
- Meningitis: Inflammation of the membranes surrounding the brain and spinal cord.
- Stroke: Shingles can increase the risk of stroke, particularly in older adults.
Prompt medical treatment is essential to prevent these complications and minimize the long-term effects of shingles. At HOW.EDU.VN, our team of doctors can provide expert care and guidance to help you manage shingles effectively and reduce the risk of complications.
8. Is Shingles Contagious? How Does It Spread?
Shingles itself is not contagious in the sense that you can’t “catch” shingles from someone who has it. However, the varicella-zoster virus (VZV), which causes shingles, can be spread to individuals who have never had chickenpox or the chickenpox vaccine. In these cases, the exposed person will develop chickenpox, not shingles.
How Shingles Spreads
The VZV virus is spread through direct contact with the fluid from shingles blisters. The virus is not spread through coughing, sneezing, or casual contact. The risk of transmission is highest when the blisters are in the active, weeping phase. Once the blisters have crusted over, the risk of transmission is significantly reduced.
Who is at Risk?
Individuals who have never had chickenpox or the chickenpox vaccine are at risk of contracting the VZV virus from someone with shingles. This includes:
- Infants: Newborns whose mothers have never had chickenpox or the vaccine are at risk.
- Children: Children who have not been vaccinated against chickenpox are susceptible.
- Adults: Adults who have never had chickenpox or the vaccine are also at risk.
Prevention Measures
If you have shingles, you can take the following steps to prevent spreading the virus to others:
- Cover the Rash: Keep the rash covered with a clean, dry bandage.
- Avoid Touching or Scratching: Avoid touching or scratching the rash to prevent spreading the virus.
- Wash Your Hands: Wash your hands frequently with soap and water, especially after touching the rash.
- Avoid Contact with Vulnerable Individuals: Avoid contact with pregnant women who have never had chickenpox, infants, and people with weakened immune systems.
- Stay Home: Stay home from work or school until the rash has crusted over.
Key Facts to Remember
- You can’t get shingles from someone who has shingles.
- You can get chickenpox from someone who has shingles if you have never had chickenpox or the chickenpox vaccine.
- The virus is spread through direct contact with the fluid from shingles blisters.
- Vaccination is the best way to prevent chickenpox and shingles.
At HOW.EDU.VN, our team of doctors can provide you with personalized advice on preventing the spread of shingles and protecting yourself and others from the varicella-zoster virus.
9. What is the Typical Duration of a Shingles Outbreak?
The typical duration of a shingles outbreak can vary, but it generally follows a predictable timeline. Understanding the stages of the illness can help you manage your symptoms and know what to expect.
Stages of a Shingles Outbreak
- Prodromal Phase (1-5 days): This is the initial phase before the rash appears. Symptoms may include pain, burning, tingling, itching, headache, fatigue, and fever.
- Active Phase (2-4 weeks): The rash appears as red bumps that turn into fluid-filled blisters. The blisters typically break open, ooze, and then crust over. The pain can be severe during this phase.
- Resolution Phase (2-4 weeks): The rash begins to heal, and the pain gradually subsides. The crusts fall off, and the skin may return to normal.
- Post-Herpetic Neuralgia (PHN): In some cases, the pain persists for months or years after the rash has healed. This is known as post-herpetic neuralgia.
Factors Affecting Duration
Several factors can affect the duration of a shingles outbreak, including:
- Age: Older adults may experience more severe symptoms and a longer duration of illness.
- Immune Status: Individuals with weakened immune systems may have a prolonged outbreak and a higher risk of complications.
- Treatment: Early treatment with antiviral medications can reduce the severity and duration of the illness.
- Complications: Complications such as bacterial infections or ophthalmic shingles can prolong the outbreak.
Average Timeline
On average, a shingles outbreak lasts for 3 to 5 weeks. However, the duration can vary depending on the individual and the factors mentioned above.
Seeking Medical Attention
If you suspect you have shingles, it’s important to seek medical attention as soon as possible. Early treatment with antiviral medications can significantly reduce the severity and duration of the illness and prevent complications.
At HOW.EDU.VN, our team of doctors can provide you with a prompt diagnosis and an individualized treatment plan to help you manage your symptoms and recover quickly from shingles.
10. When Should I Consult a Doctor or Specialist for Shingles?
Consulting a doctor or specialist promptly is crucial for managing shingles effectively and preventing potential complications. Here are several situations when you should seek medical attention:
Early Symptoms
If you experience any early symptoms of shingles, such as pain, burning, tingling, or itching on one side of your body, it’s important to consult a doctor as soon as possible. Early treatment with antiviral medications can significantly reduce the severity and duration of the illness.
Rash Development
If you develop a rash that resembles shingles, characterized by red bumps that turn into fluid-filled blisters on one side of your body, seek medical attention immediately. A doctor can confirm the diagnosis and initiate appropriate treatment.
Severe Pain
If you experience severe pain associated with the shingles rash, consult a doctor or pain specialist. Effective pain management is essential for improving your quality of life and preventing chronic pain.
Eye Involvement
If the shingles rash affects your eye or the area around your eye, seek immediate medical attention from an ophthalmologist. Ophthalmic shingles can lead to serious eye complications, including vision loss.
Weakened Immune System
If you have a weakened immune system due to conditions such as HIV/AIDS, cancer, or immunosuppressant medications, you are at higher risk of developing severe shingles and complications. Consult a doctor promptly for specialized care.
Pregnancy
If you are pregnant and suspect you have shingles, seek medical attention immediately. Shingles during pregnancy can pose risks to both the mother and the baby.
Lack of Improvement
If your symptoms do not improve with home remedies or over-the-counter medications, consult a doctor. You may need prescription medications or other medical interventions.
Signs of Infection
If the shingles rash shows signs of infection, such as increased redness, swelling, pus, or fever, seek medical attention promptly. Bacterial infections can lead to serious complications.
Persistent Pain After Rash Heals
If you experience persistent pain for months or years after the shingles rash has healed, consult a doctor or pain specialist. This condition, known as post-herpetic neuralgia (PHN), requires specialized treatment.
Neurological Symptoms
If you experience neurological symptoms such as facial paralysis, hearing loss, vertigo, or confusion, seek immediate medical attention. These symptoms may indicate Ramsay Hunt syndrome or other serious complications.
Expert Care at HOW.EDU.VN
At HOW.EDU.VN, we understand the challenges of dealing with shingles and its complications. Our team of experienced doctors and specialists is dedicated to providing you with the highest quality care and support. We offer:
- Prompt Diagnosis: We provide quick and accurate diagnoses to ensure timely treatment.
- Individualized Treatment Plans: We develop personalized treatment plans tailored to your specific needs and symptoms.
- Pain Management: We offer effective pain management strategies to alleviate your discomfort and improve your quality of life.
- Specialized Care: We provide specialized care for ophthalmic shingles, Ramsay Hunt syndrome, and other complications.
- Vaccination: We offer shingles vaccination to prevent future outbreaks.
- Support and Education: We provide you with the information and resources you need to manage shingles effectively.
Don’t let shingles control your life. Contact us today at HOW.EDU.VN to schedule a consultation and receive the expert care you deserve. Our address is 456 Expertise Plaza, Consult City, CA 90210, United States. You can also reach us via Whatsapp at +1 (310) 555-1212.
 Shingles Home Remedies
Shingles Home Remedies
FAQ About Shingles Treatment
Here are some frequently asked questions about shingles treatment:
1. What is the most effective treatment for shingles?
The most effective treatment for shingles involves antiviral medications such as acyclovir, valacyclovir, or famciclovir, started within 72 hours of the rash appearing. Pain management is also crucial.
2. Can shingles be cured completely?
No, shingles cannot be cured completely, but antiviral medications can reduce the severity and duration of the illness and prevent complications.
3. How long does it take for shingles to heal with treatment?
With treatment, the shingles rash typically heals within 2 to 4 weeks. However, pain may persist for longer in some cases.
4. What can I do to relieve the pain of shingles?
Pain relief measures include over-the-counter pain relievers, prescription pain medications, topical treatments, and nerve pain medications.
5. Are there any home remedies that can help with shingles?
Yes, home remedies such as cool compresses, colloidal oatmeal baths, calamine lotion, and honey can help relieve shingles symptoms.
6. Is the shingles vaccine effective in preventing shingles?
Yes, the Shingrix vaccine is highly effective in preventing shingles and post-herpetic neuralgia.
7. Can I get shingles more than once?
Yes, it is possible to get shingles more than once, although it is less common.
8. What are the risk factors for developing shingles?
Risk factors include age over 50, weakened immune system, stress, and certain medical conditions.
9. Is shingles contagious?
Shingles itself is not contagious, but the varicella-zoster virus can be spread to individuals who have never had chickenpox or the chickenpox vaccine.
10. When should I see a doctor for shingles?
You should see a doctor as soon as possible if you experience any symptoms of shingles, especially if you are pregnant, have a weakened immune system, or have eye involvement.
For expert advice and personalized treatment for shingles, contact our team of doctors at how.edu.vn. We are here to help you manage your symptoms, prevent complications, and improve your quality of life. Address: 456 Expertise Plaza, Consult City, CA 90210, United States. Whatsapp: +1 (310) 555-1212.