Kidney transplantation stands as the preferred treatment for End-Stage Kidney Disease (ESKD), offering improved survival rates and a better quality of life compared to dialysis. The first successful kidney transplant in the United States, performed in 1954 by Dr. Joseph Murray, paved the way for the widespread adoption of this life-saving procedure after the Uniform Anatomic Gift Act of 1968 allowed US adults to donate their organs. This article will explore the current state of kidney transplantation in adults in the United States, focusing particularly on the costs associated with the procedure, post-transplant outcomes, and existing barriers.
The Process of Organ Allocation
Unlike transplants of other solid organs like the liver and heart, kidney allocation primarily hinges on waiting time rather than the severity of the patient’s condition. However, candidates also accrue points for prior living donation, a higher calculated panel reactive antigen score, and the extent of human leukocyte antigen-DR mismatch. The higher the allocation score, the higher the candidate’s position on the waitlist. In the United States, patients become eligible for waitlisting once their eGFR (estimated glomerular filtration rate) reaches ≤20 ml/min per 1.73 m2. Allocation policies underwent significant revisions in December 2014 to address disparities in early referral for kidney transplants, which disproportionately affected non-White patients. Further changes in March 2021 aimed to reduce geographic disparities in transplant access, moving from Donation Service Area boundaries to proximity circles from the deceased donor organ.
Recipient Evaluation and Wait Times
Across the United States, 256 kidney transplant programs evaluate candidates referred by their nephrologists through rigorous medical and psychosocial assessments. If approved, patients are placed on a national waitlist managed by the Organ Procurement and Transplantation Network. Currently, 92,751 patients are on the waitlist for a kidney alone or a kidney-pancreas transplant in the United States, representing only 18% of prevalent patients on dialysis. The average wait time for a deceased donor kidney transplant is 5 years but can vary depending on the listing region and blood type. Unfortunately, more than half of listed candidates either die or are removed from the list before receiving a transplant.
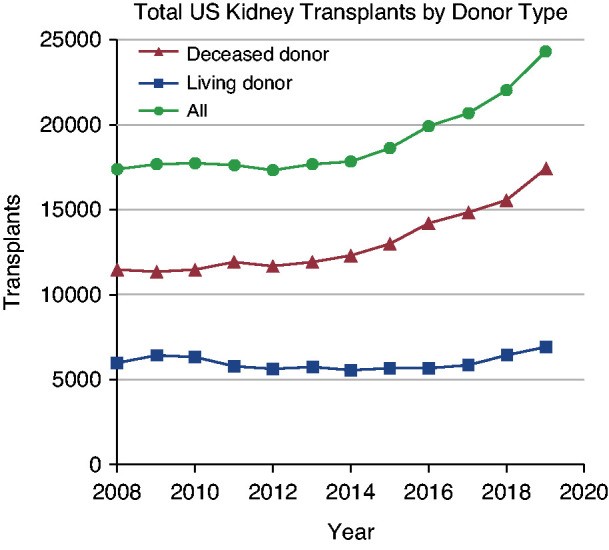
Kidney Transplant Statistics
As of December 2018, there were 229,887 patients in the United States with a functioning kidney transplant, or 678 recipients per million people, representing a 40% growth since 2008. In 2019, a record 24,273 kidney transplants were performed in the United States. Approximately 72% of these transplants came from deceased donors. The recipients were primarily men (61%), and half had either diabetes mellitus (30%) or hypertension (20%) as the listed cause of ESKD, whereas glomerulonephritis (GN) (18%) and cystic kidney disease (13%) were less common. Non-Hispanic White patients comprised the largest proportion of transplant recipients (45%), followed by Black (27%), Hispanic (19%), and Asian (7%) participants. The trend of increasing transplants in patients aged 50–64 years and ≥65 years relative to other age groups has continued since 2015, with those aged ≥50 accounting for 60% of transplant recipients in 2019. Racial disparities in access to living donor kidney transplant have persisted and worsened over the past two decades. Referral and waitlisting disparities also persist.
Immediate Post-Transplant Care
In the United States, highly trained transplant surgeons, having completed specialized fellowship training, perform kidney transplant surgeries. The average hospital stay post-transplant is 6.7 days (ranging from 4 to 7 days). Following discharge, care is managed in an outpatient setting by transplant nephrologists and surgeons, alongside clinical pharmacists, social workers, and transplant nurse coordinators, depending on the institution. Patients living far from the transplant center may choose to return to their general nephrologist for primary transplant management after the initial post-transplant period.
Almost all kidney transplant recipients in the United States receive induction therapy. T cell–depleting agents have increased in use over the past 10 years and are given to 74% of patients, whereas 21% receive an IL-2 receptor antagonist. A triple regimen of tacrolimus, mycophenolate mofetil, and corticosteroids is the predominant initial maintenance immunosuppression and is given to 65% of patients. While a quarter of recipients receive steroid-free immunosuppressive regimens, this percentage has remained stable over the past decade.
Kidney Transplantation Costs: Breaking Down the Expenses
The question everyone asks is: How Much Does A Kidney Transplant Cost? In 2020, the average kidney transplant cost in the United States was approximately US$442,500. The transplant admission itself, encompassing the surgery, constitutes the most significant expense, accounting for 34% of the total cost. Immunosuppression and other transplant-related medications, such as prophylactic antibiotics (from the time of transplant to 6 months post-transplant), account for only 7% of the total costs, despite rising medication prices. Understanding these costs is crucial for patients and their families as they navigate the transplant process.
Insurance Coverage and Financial Aid
In 2019, the majority of transplant recipients had public Medicare coverage (60%) compared with private insurance (32%). A smaller percentage had Medicaid (6%), a state-run program for low-income individuals, or other government insurance (2%). Although Medicare is generally available to individuals aged ≥65 years, patients with ESKD in the United States are automatically eligible. Medicare coverage includes the pretransplant workup, perioperative inpatient care, provider professional fees, and immunosuppression. However, Medicare typically only covers 80% of costs, necessitating a secondary policy to cover the remainder. Furthermore, Medicare eligibility ends at 3 years post-transplant unless the recipient is aged ≥65 years or disabled. To address the issue of allograft failures due to lack of access to immunosuppression, the US Congress passed the Comprehensive Immunosuppressive Drug Coverage for Kidney Transplant Patients Act in December 2020. This law, effective in 2023, extends Medicare immunosuppression coverage for the life of the transplant. This is a significant step in ensuring long-term care and reducing the financial burden on transplant recipients.
Excellent Outcomes and Survival Rates
Both short- and long-term allograft and patient survival rates in the United States are excellent and have steadily improved over the past decade. Unadjusted death-censored allograft survival rates in deceased donor kidney transplant recipients were 97%, 90%, and 77% at 1, 5, and 10 years, respectively. Living donor transplant recipients have even better unadjusted death-censored allograft survival rates compared with their deceased donor counterparts, with 1, 5, and 10-year rates of 99%, 94%, and 84%, respectively. A similar trend was seen in patient survival. For patients transplanted in 2013, the unadjusted 1, 5, and 10-year patient survival rates in living donor recipients were 99%, 94%, and 85%, respectively, compared with 99%, 89%, and 75%, respectively, in deceased donor recipients.
Future Objectives and Challenges
The Advancing American Kidney Health initiative, launched in July 2019, outlined several goals to improve the care of patients with Chronic Kidney Disease (CKD) in the United States. One of the initiative’s key objectives was to improve access to kidney transplantation by: (1) doubling the number of kidneys available for transplant by 2030, (2) increasing procurement and reducing discards of deceased donor organs, and (3) reducing disincentives and providing financial incentives to living organ donation.
The primary obstacle to achieving these goals remains the shortage of donors. Although the number of kidney transplants performed in the United States was 30% higher in 2019 compared with 2015, this was still insufficient to meet the demand, as evidenced by the roughly 90,000 patients currently waitlisted for transplant. Consequently, wait times in the United States are lengthening, especially for those with O or B blood types, and many waitlisted candidates will die or become too sick to undergo transplant. The transplant community is discussing incentivizing the transplantation of “nonstandard” kidneys to reduce the deceased donor organ discard rate when the survival benefits outweigh the risk of remaining on dialysis. Direct-acting antivirals for hepatitis C have also significantly decreased the discard rate of hepatitis C antibody–positive kidneys procured for transplant.
Expanded utilization of deceased donor kidneys will not be sufficient to address the need to increase the donor pool. Despite a slight upward trend since 2018, the number of living donor transplants performed annually has remained stagnant over the past decade. Intensifying strategies to encourage living donation, particularly among non-White candidates, is crucial. Living donors often incur significant donation-related expenses not covered by the recipient’s health insurance, and financial burdens are frequently cited as a barrier. Since October 22, 2020, the US Department of Health and Human Services now allows living donors to be reimbursed for lost wages, child care expenses, and elder care expenses.
Kidney transplantation has become widely accessible in the United States over many decades, with improving allograft and patient post-transplant outcomes. Nonetheless, several challenges persist. Increasing living donation, reducing the wait time for transplants, and eliminating racial disparities in access to transplant are all future priorities for the US transplant community. Understanding how much a kidney transplant costs and the available financial aid options is a critical component of addressing these challenges and ensuring more patients can access this life-saving procedure.