Considering hormone replacement therapy (HRT) can bring a wave of excitement, imagining relief from hot flashes, better sleep, and a return to your old self during perimenopause, menopause, and beyond. But a crucial question often arises: “How Much Is Hrt going to cost me?” This guide breaks down the costs associated with HRT, exploring different options, insurance coverage, and ways to make it more affordable.
Breaking Down the Cost of Hormone Replacement Therapy
The price of hormone replacement therapy, like any prescription medication, depends on several key factors:
- Type of HRT: Different forms of HRT have varying costs.
- Brand Name vs. Generic: Generic medications are typically significantly cheaper than brand-name versions.
- Insurance Coverage: Your prescription drug coverage can significantly reduce your out-of-pocket expenses.
- Dosage and Treatment Regimen: The dosage and specific combination of hormones prescribed will influence the overall cost.
HRT Options and Their Price Ranges
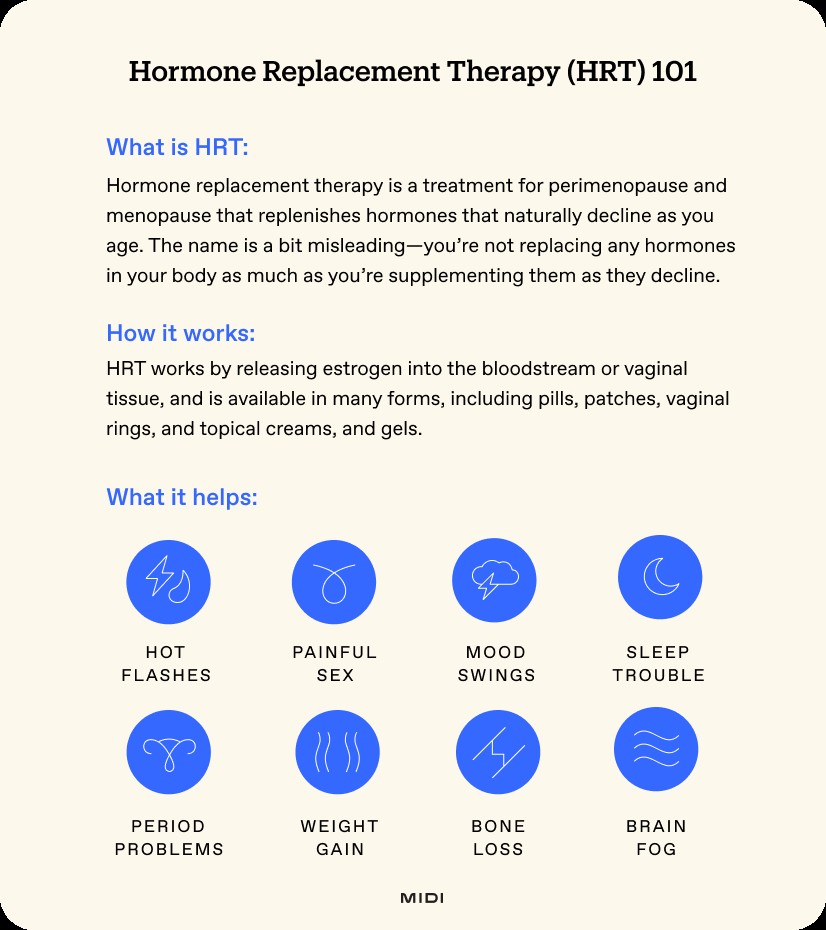
Hormone replacement therapy (HRT), also known as menopausal hormone therapy (MHT), supplements declining hormone levels, primarily estrogen and progesterone, during perimenopause and menopause. While it’s called “replacement,” it’s more about supplementing these hormones as your body produces less of them. HRT effectively manages menopause symptoms caused by these hormonal fluctuations.
Choosing the right HRT can feel overwhelming. Consulting a healthcare professional, like those at Midi Health, helps you navigate these options and find a treatment plan that suits your lifestyle, medical history, symptoms, and budget. Many HRT medications are covered by insurance, so it’s wise to check your plan’s coverage and copays.
Here’s a breakdown of common HRT options and their general cost ranges:
HRT Pills
What they are: Oral estrogen pills are a common form of HRT. Estrace and Premarin are frequently prescribed, and are also available as creams. Some women in perimenopause may use birth control pills for symptom management and contraception. Note that HRT is not a contraceptive.
How they work: Typically taken once daily, though dosage schedules may vary based on your individual treatment plan.
Why you should consider them: Pills are a suitable option for those who prefer not to use other forms of HRT. Oral estrogen and progesterone are as effective as patches in alleviating hot flashes and night sweats, according to The Menopause Society. However, estrogen pills can interfere with thyroid levels and increase the risk of clotting issues. They should be avoided by women with cardiovascular risk factors like heart disease.
Potential side effects: Abdominal pain, breast tenderness, back pain, headaches, increased blood pressure, and nausea.
What they cost: Generic pills can cost less than $10 for a 90-day supply, while brand-name options can exceed $500.
HRT Patches
What they are: Hormone replacement patches, also called estradiol patches, are applied to the skin. They are a popular first-line therapy due to milder side effects than pills. Patches come in estrogen-only (estradiol) or combination (estrogen and progesterone) forms.
How they work: Estradiol patches (e.g., Alora, Minivelle, Vivelle-Dot, Climara) are typically applied once or twice a week to clean, dry skin on the lower abdomen. Change the location slightly each time for best absorption.
Why you should consider them: Patches bypass the liver and have lower clotting risks than pills, making them suitable for women with cardiovascular risk factors like DVT, hypercholesterolemia, hypertension, or diabetes. They’re also a good choice for women starting HRT after age 60. Patches can also help prevent osteoporosis.
Potential side effects: Skin irritation, breast tenderness, vaginal discharge, and nausea.
What they cost: With insurance, a month’s supply of patches can cost less than $40, but without insurance, it can exceed $250.
Vaginal Estrogen Creams
What they are: Estrace and Premarin are available as vaginal creams.
How they work: Creams are inserted into the vagina several times per week, delivering estrogen directly to the vulva and vagina.
Why you should consider them: Vaginal estrogen creams are effective for relieving vaginal dryness and irritation, eliminating symptoms of vaginal atrophy in 80-90% of cases. They directly supply estrogen to the vaginal tissues, unlike moisturizers and lubricants which only temporarily ease irritation.
Potential side effects: Vaginal discharge, irregular bleeding, yeast infections, and breast tenderness.
What it costs: $25 – $100 per month, with some insurers covering them completely.
Vaginal Rings
What they are: Rings are inserted into the upper vagina to deliver hormones locally. Lower-dose rings (Estring) provide local estrogen therapy for menopausal changes in and around the vagina, while higher-dose rings (Femring) deliver systemic estradiol for vasomotor symptoms like hot flashes.
How they work: Rings slowly release hormones locally to the vagina and are typically replaced every 90 days.
Why you should consider them: Lower-dose rings target vaginal dryness and irritation, while higher doses also help ease hot flashes and night sweats.
Potential side effects: Headaches, spotting, bloating, back pain, and urinary tract infections (UTIs).
What they cost: About $500 or more per ring out of pocket. With insurance, the price can drop to less than $30, though insurers may require trying other regimens first.
Vaginal Suppositories
What they are: Vaginal tablets (Vagifem) or suppositories (Imvexxy) are inserted into the vagina to deliver hormones locally.
How they work: Tablets or suppositories slowly release hormones locally. Initially, daily insertion may be required, then doses are spread out over time.
Why you should consider them: Tablets can alleviate vaginal symptoms like dryness, irritation, or burning. Depending on the dose, they may also help with hot flashes and night sweats.
Potential side effects: Vaginal discharge, irregular bleeding, and yeast infections.
What they cost: Generics can be found for $40 or less per pack, while brand names can exceed $200 out of pocket.
Gels
What they are: Topical gels (Divigel, Elestrin, Estrogel, Estroge) are applied topically, with each type applied slightly differently (arm or thigh).
How they work: Applied once daily, estrogen is absorbed through the skin into the bloodstream, providing a steady release, similar to patches.
Why you should consider them: Gels effectively treat hot flashes and night sweats. Estrogel can also help with vaginal dryness and burning. Gels are suitable for those who prefer not to take pills, have adverse reactions to patches, or experience side effects with either medication. Like patches, gels may also be safer than pills for women with cardiovascular risk factors, but aren’t as extensively studied.
Potential side effects: Vaginal discharge, irregular bleeding, yeast infections, headaches, and breast tenderness.
What they cost: Generic brands can cost less than $50 for a 30-day supply, while some varieties cost more than $200. Insurance may cover gels if you’ve had an allergic reaction to patch adhesives.
Pellets
What they are: Hormone pellets are small capsules implanted in the body by a healthcare professional every three to six months, usually containing a mix of estrogen and testosterone.
How they work: Inserted hormones are released directly into the bloodstream.
Why you should consider them: Some women report improved sleep, libido, and fewer hot flashes. However, many doctors, including Midi clinicians, don’t recommend them due to a lack of evidence around their safety and efficacy. Removing them is difficult, which means patients must wait for them to stop working if the dose is too high or there’s a bad reaction.
Potential side effects: High doses of testosterone pellets can cause acne, oily skin, increased facial or body hair, voice changes (which can be irreversible), and mood changes.
What they cost: Pellet treatments are not FDA-approved and aren’t covered by insurance, costing about $1,500 annually.
Progesterone Pills, Patches, and Creams
What they are: Progesterone is often used alongside estrogen in HRT. Oral progesterone is the first-line recommendation, but it can also be administered via patch or cream (though vaginal progesterone creams have less research supporting their efficacy).
How they work: Progesterone reduces the risk of uterine cancer by preventing the thickening of the uterine lining caused by estrogen. It may be taken daily with estrogen or only on certain days of the month.
Why you should consider them: If you have a uterus and are prescribed estrogen as part of your HRT, progesterone is typically included to reduce the risk of uterine cancer. Some patients who have had a hysterectomy may still be counseled to include progesterone to help with sleep and insomnia.
Potential side effects: Peanut allergies may preclude certain types of progesterone (progesterone capsules contain peanut oil). Other side effects can include bloating, breast tenderness, fatigue, irregular bleeding, diarrhea, and mood changes.
What they cost: Less than $20 for a 90-day supply, but can be more depending on brand and dosage.
Testosterone Creams and Gels
What they are: Testosterone creams and gels can help with decreases in libido and arousal, and many patients report improvements in other symptoms like brain fog, insomnia, muscle mass, and energy.
How they work: Testosterone levels decline during the menopause transition. While not FDA-approved for women, it’s often prescribed as a compounded cream applied to the thigh. Some doctors may prescribe testosterone gels (Testim or Androgel) off-label at a much lower dosage than what is given to men.
Why you should consider them: Testosterone may be a solution for low libido, particularly in post-menopausal women. It has also been reported to help with energy, muscle mass, concentration, and sleep, though research is still evolving on why.
Potential side effects: Acne, increased facial hair, weight gain, and deepening of the voice.
What it costs: Testosterone is not typically covered by insurance and can range from $45 for a 30-day supply to $100+ for a 90-day supply out of pocket. Additional labs and follow-up visits may be required, which can add additional costs.
Navigating HRT Costs: Insurance and Savings
Is Hormone Replacement Therapy Covered By Insurance?
Many FDA-approved HRT options are covered by private insurance. Confirm coverage with your provider.
Is Hormone Replacement Therapy Safe?
HRT is considered safe. Research shows that women starting HRT within 10 years of their last period experience relief from menopausal symptoms and have a lower risk of heart disease and bone loss. HRT may also decrease the risk of diabetes and weight gain.
Is Hormone Replacement Therapy Covered By Medicare and Medicaid?
Medicare Part D can cover HRT meds, and some Medicare Part C plans include drug coverage. However, each plan has its own list of covered meds, so confirm which forms and brands of HRT are covered.
Many state Medicaid programs cover HRT, but not all. Check your coverage to confirm.
How Can I Save on Hormone Replacement Therapy?
If your HRT meds aren’t covered by insurance, ask your pharmacy about the “cash price,” which is often discounted. Pharmaceutical companies may offer savings cards, and GoodRx provides coupons.
What Are Alternatives to Hormone Replacement Therapy?
HRT isn’t the only option. Consider these alternatives:
- Lifestyle choices: Physical activity, diet changes, better sleep strategies, mindfulness, cognitive behavioral therapy, and acupuncture.
- Supplements and botanicals: Black cohosh for hot flashes; red clover for bone and cardiovascular health; ashwagandha for mood swings and anxiety.
- Non-hormonal prescriptions: Low-dose SSRIs, blood pressure medications, anti-seizure medications, and overactive bladder meds. Weight-loss meds, like GLP-1s, can also help with midlife weight gain.
Final Thoughts on HRT Costs
Hormone replacement therapy offers a range of options to suit different needs and budgets, with costs spanning from $10 to over $500 per month. Consulting a healthcare professional is essential to determine if HRT is the right choice and to receive personalized recommendations based on your symptoms, lifestyle, and medical history.
Many women experience significant symptom improvement with HRT:
![Testimonial about HRT relieving joint pain and hot flashes]
![Testimonial about feeling different after a few weeks on HRT]
Taking the first step and consulting with a clinician ensures that you find the most effective and affordable option for relief.
Cagnacci, A., & Venier, M. (2019). The Controversial History of Hormone Replacement Therapy. Medicina, 55(9). https://doi.org/10.3390/medicina55090602
Cancer of the Endometrium – Cancer Stat Facts. (2018). National Cancer Institute – SEER. https://seer.cancer.gov/statfacts/html/corp.html
Harper-Harrison, G., & Shanahan, M. M. (2023, February 20). Hormone replacement therapy. National Library of Medicine; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK493191/
North American Menopause Society. (2022). The 2022 hormone therapy position statement of The North American Menopause Society. Menopause (New York, N.Y.), 29(7), 767–794. https://doi.org/10.1097/GME.0000000000002028
What Medicare Part D drug plans cover | Medicare. (2019). Medicare.gov. https://www.medicare.gov/drug-coverage-part-d/what-medicare-part-d-drug-plans-cover