Navigating the world of newborn feeding can be both exciting and overwhelming. Understanding exactly how much a 2-month-old should eat in 24 hours is crucial for their healthy development. At HOW.EDU.VN, our panel of expert pediatricians and lactation consultants provide insights and personalized guidance to help you confidently meet your baby’s nutritional needs. Learn about infant feeding guidelines, growth spurts, and feeding cues.
1. Understanding Newborn Feeding Patterns at 2 Months
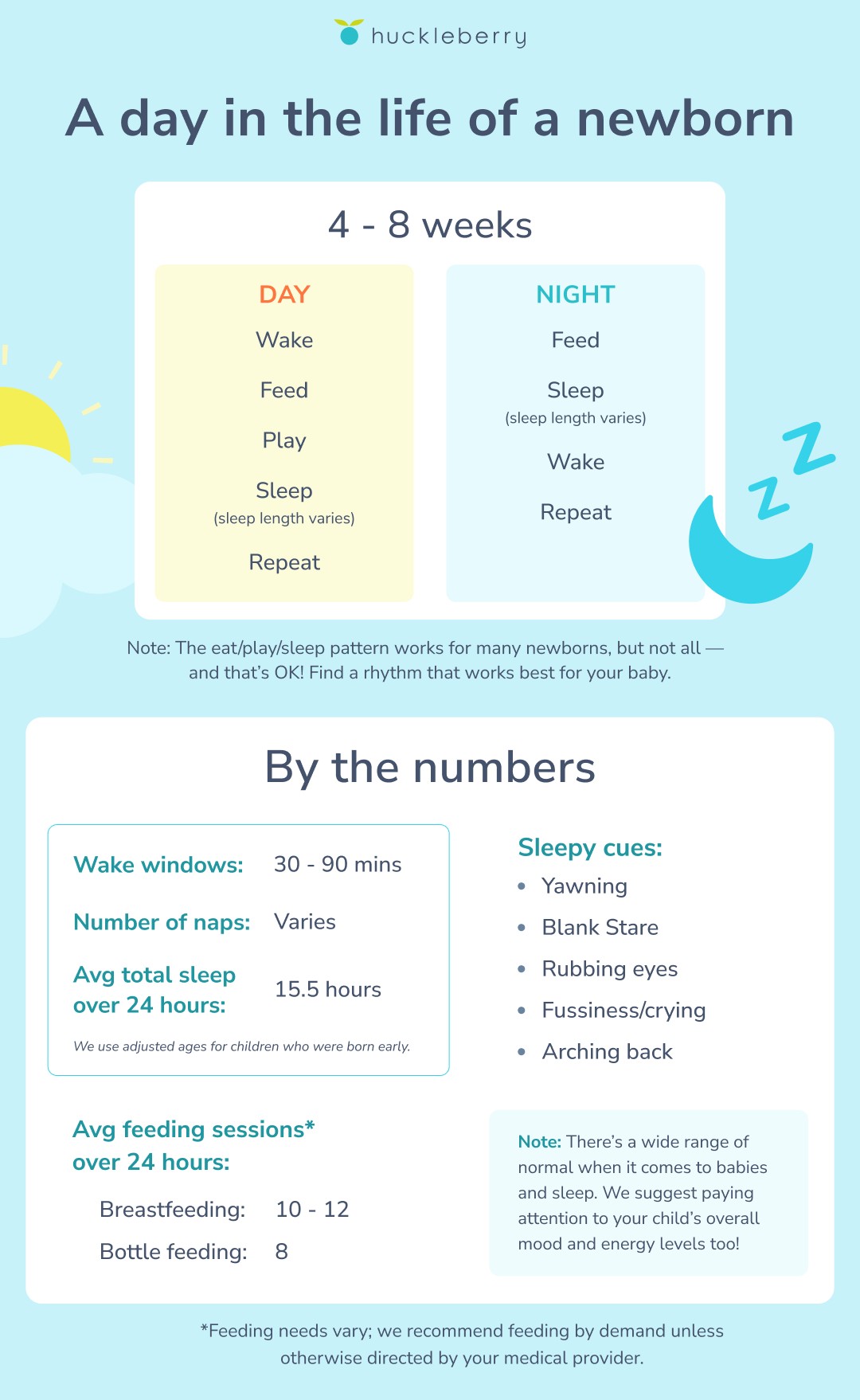
At the 2-month mark, your baby is likely developing more consistent feeding habits. While every baby is different, understanding general feeding patterns can help you gauge whether your little one is getting enough nourishment. The American Academy of Pediatrics recommends responsive feeding, often referred to as feeding on demand, which means paying close attention to your baby’s hunger cues rather than adhering strictly to a schedule. This approach ensures that your baby gets the right amount of food based on their individual needs.
 Newborn sleep schedule
Newborn sleep schedule
2. How Much Should Your 2-Month-Old Baby Eat?
Typically, a 2-month-old baby will eat every 2 to 4 hours. Breastfed babies often feed more frequently because breast milk is digested more quickly than formula. At each feeding, newborns at this age usually consume about 3 to 4 ounces, resulting in approximately 8 to 12 feedings within a 24-hour period. However, it is essential to remember that these are just averages, and your baby’s individual needs may vary.
2.1. Breast Milk vs. Formula
Breast milk and formula provide the necessary nutrients for your growing baby, but there are differences in how they are digested. Breast milk is easier to digest, so breastfed babies tend to eat more often. Formula-fed babies may go slightly longer between feedings as formula takes more time to digest.
2.2. Tracking Your Baby’s Feedings
Monitoring your baby’s feeding habits can provide valuable insights into their nutritional intake. Consider using a baby tracking app or simply keeping a log to record feeding times, amounts, and any relevant notes. This information can be helpful when discussing your baby’s feeding habits with their pediatrician or a lactation consultant.
3. Key Indicators: Is Your Baby Getting Enough?
Determining whether your 2-month-old is getting enough to eat involves looking at a combination of factors, including weight gain, diaper output, and behavior. These indicators can provide a comprehensive view of your baby’s nutritional status.
3.1. Weight Gain
One of the most reliable indicators of adequate nutrition is consistent weight gain. During the first few months, babies typically gain about 4 to 7 ounces per week. Your pediatrician will monitor your baby’s weight at regular check-ups to ensure they are on track.
3.2. Diaper Output
Diaper output is another critical indicator. A well-hydrated and adequately fed 2-month-old should have at least 5 to 6 wet diapers and several bowel movements each day. Changes in diaper output could signal that your baby isn’t getting enough fluids or nutrients.
3.3. Behavioral Cues
Pay attention to your baby’s behavior. A satisfied baby is generally content and alert after feedings. If your baby seems fussy, restless, or constantly hungry, it could indicate that they need more milk or formula.
4. Tips for Successful Feeding
Feeding your 2-month-old can be a rewarding experience, but it can also present challenges. Here are some practical tips to help ensure successful feedings and promote your baby’s healthy development.
4.1. Recognize Hunger Cues
Learning to recognize your baby’s hunger cues is essential for responsive feeding. Common hunger cues include:
- Licking lips
- Sucking on hands or fingers
- Rooting (turning their head and opening their mouth as if searching for the nipple or bottle)
- Fussiness or restlessness
Addressing these cues promptly can help prevent your baby from becoming overly hungry and frustrated.
4.2. Create a Calm Environment
A calm and quiet environment can help your baby focus on feeding. Minimize distractions by turning off the TV, dimming the lights, and finding a comfortable position for both you and your baby. This can make the feeding process more enjoyable for both of you.
4.3. Proper Latch and Positioning
For breastfeeding mothers, proper latch and positioning are crucial for successful feeding and preventing nipple pain. Ensure that your baby is latching deeply onto the areola, not just the nipple. Experiment with different breastfeeding positions to find one that is comfortable for both you and your baby.
4.4. Burping Your Baby
Burping your baby during and after feedings can help release trapped air and prevent discomfort. Gently pat or rub your baby’s back while holding them upright or over your shoulder.
5. Addressing Common Feeding Challenges
Many parents encounter feeding challenges with their 2-month-olds. Understanding these challenges and how to address them can make the feeding process smoother and more enjoyable.
5.1. Refusal to Feed
If your baby suddenly refuses to feed, it could be due to various factors, such as illness, teething, or a change in routine. Consult with your pediatrician to rule out any medical issues.
5.2. Spitting Up
Spitting up is common in newborns and is usually not a cause for concern. However, frequent or forceful vomiting could indicate a problem, such as gastroesophageal reflux. Consult with your pediatrician if you are concerned about your baby’s spitting up.
5.3. Colic
Colic, characterized by excessive crying and fussiness, can be challenging for both parents and babies. While the exact cause of colic is unknown, various strategies, such as swaddling, gentle rocking, and using a pacifier, may help soothe your baby.
6. The Role of Night Feedings
Night feedings are a normal and necessary part of newborn care. At 2 months old, babies still have small stomachs and require frequent feedings to support their rapid growth and development.
6.1. Why Night Feedings Are Important
Night feedings provide essential calories and nutrients that your baby needs to grow and thrive. They also help regulate your milk supply if you are breastfeeding.
6.2. Managing Night Feedings
While night feedings are necessary, they can be exhausting for parents. Try to create a consistent bedtime routine, feed your baby in a dimly lit room, and minimize stimulation during night feedings to help them fall back asleep more easily.
6.3. When to Reduce Night Feedings
As your baby gets older, they may gradually start sleeping for longer stretches at night and require fewer night feedings. Consult with your pediatrician to determine when it is appropriate to reduce or eliminate night feedings.
7. Growth Spurts and Feeding
Growth spurts are periods of rapid growth that typically occur around 2 weeks, 6 weeks, 3 months, and 6 months of age. During a growth spurt, your baby may seem hungrier than usual and want to feed more frequently.
7.1. Recognizing Growth Spurts
Common signs of a growth spurt include increased hunger, fussiness, and changes in sleep patterns. Be prepared to offer extra feedings during these periods to meet your baby’s increased needs.
7.2. Adjusting Feeding Amounts
During a growth spurt, it’s essential to adjust the amount of breast milk or formula you offer to satisfy your baby’s increased appetite. Trust your baby’s cues and feed them on demand.
8. Expert Advice from HOW.EDU.VN’s Pediatricians
Navigating newborn feeding can be complex, and it’s natural to have questions and concerns. At HOW.EDU.VN, we offer access to a team of experienced pediatricians and lactation consultants who can provide personalized guidance and support.
8.1. When to Seek Professional Help
If you have concerns about your baby’s feeding habits, weight gain, or overall health, don’t hesitate to seek professional help. Our experts can assess your baby’s individual needs and provide tailored recommendations.
8.2. Personalized Feeding Plans
Our pediatricians can develop personalized feeding plans based on your baby’s specific needs and circumstances. These plans take into account factors such as your baby’s age, weight, medical history, and feeding preferences.
8.3. Lactation Support
For breastfeeding mothers, our lactation consultants offer comprehensive support and guidance. They can help you with latch issues, milk supply concerns, and other breastfeeding challenges.
9. Understanding Hunger and Fullness Cues
One of the most important aspects of responsive feeding is understanding your baby’s hunger and fullness cues. This allows you to feed your baby when they are truly hungry and avoid overfeeding.
9.1. Recognizing Hunger Cues
Hunger cues can be subtle at first, but with practice, you’ll become more adept at recognizing them. Common hunger cues include:
- Early Cues: Stirring, opening their mouth, turning their head as if looking for the breast or bottle (rooting reflex), bringing hands to their mouth.
- Active Cues: Stretching, increased physical movement, fussiness, and eventually, crying. Crying is often a late hunger cue, so it’s best to respond to earlier cues to avoid an upset baby.
9.2. Recognizing Fullness Cues
Just as important as recognizing hunger cues is knowing when your baby is full. Fullness cues indicate that your baby has had enough to eat and is satisfied. Common fullness cues include:
- Slowing Down: Pausing frequently during feeding, losing interest in sucking.
- Turning Away: Turning their head away from the breast or bottle.
- Closing Mouth: Keeping their mouth closed or pushing the nipple/bottle out of their mouth.
- Relaxation: Relaxing their hands, appearing sleepy or content.
- Spitting Out: Spitting out the nipple or bottle, indicating they no longer want to feed.
9.3. Responsive Feeding Practices
Responsive feeding means paying attention to these cues and responding appropriately. This approach helps your baby develop healthy eating habits and a positive relationship with food. Avoid forcing your baby to finish a bottle or breast if they are showing signs of fullness.
10. Addressing Fussiness and Crying
Fussiness and crying are common behaviors in newborns, and they don’t always indicate hunger. It’s essential to consider other possible reasons for fussiness before assuming your baby is hungry.
10.1. Common Reasons for Fussiness
- Tiredness: Newborns can become easily overstimulated and tired.
- Discomfort: Diaper rash, gas, or being too hot or cold can cause discomfort.
- Overstimulation: Too much noise, light, or activity can overwhelm a newborn.
- Need for Comfort: Sometimes babies simply want to be held and cuddled.
10.2. Soothing Techniques
If your baby is fussy but doesn’t seem hungry, try these soothing techniques:
- Swaddling: Wrapping your baby snugly in a blanket can provide a sense of security.
- Gentle Rocking: Rocking your baby gently can be calming.
- White Noise: Soft, continuous sounds like a fan or white noise machine can be soothing.
- Skin-to-Skin Contact: Holding your baby against your bare chest can promote bonding and relaxation.
- Pacifier: Offering a pacifier can help soothe a fussy baby.
10.3. Knowing When to Feed
If you’ve ruled out other causes of fussiness and your baby is showing hunger cues, it’s time to offer a feeding. Trust your instincts and respond to your baby’s needs.
11. Understanding Nursing Strikes
A nursing strike is when a baby who has been breastfeeding well suddenly refuses to nurse. This can be distressing for mothers, but it’s usually temporary and often related to an identifiable cause.
11.1. Common Causes of Nursing Strikes
- Illness: A stuffy nose, ear infection, or sore throat can make it difficult or uncomfortable for a baby to nurse.
- Teething: Teething pain can make babies reluctant to nurse.
- Stress: Changes in routine, travel, or other stressors can affect a baby’s willingness to nurse.
- Change in Milk Taste: Changes in the mother’s diet, medications, or menstruation can alter the taste of breast milk.
- Discomfort: A change in nursing position, pressure on the baby’s head, or a forceful let-down can cause discomfort.
11.2. Strategies for Managing Nursing Strikes
- Rule Out Medical Issues: Consult with your pediatrician to rule out any underlying medical causes.
- Offer Comfort: Provide extra cuddles and skin-to-skin contact.
- Pump and Feed: Pump your breast milk and offer it to your baby in a bottle or cup. This ensures they are still getting breast milk while you address the nursing strike.
- Nurse When Sleepy: Try nursing your baby when they are sleepy or drowsy, as they may be more willing to latch on.
- Change Nursing Position: Experiment with different nursing positions to see if one is more comfortable for your baby.
- Stay Patient: Nursing strikes are usually temporary, so stay patient and continue to offer the breast.
11.3. When to Seek Help
If the nursing strike lasts for more than a few days or you are concerned about your baby’s intake, consult with a lactation consultant or your pediatrician. They can help identify the cause of the nursing strike and provide guidance on how to resolve it.
12. Is My Baby Eating Too Much or Too Little?
Parents often worry about whether their baby is eating the right amount. While there’s a range of normal, here are some general guidelines to help you assess whether your baby is getting enough or too much.
12.1. Signs of Adequate Intake
- Weight Gain: Consistent weight gain is one of the best indicators of adequate intake. Babies typically gain about 4 to 7 ounces per week in the first few months.
- Diaper Output: A well-hydrated baby should have at least 5-6 wet diapers and several bowel movements each day.
- Contentment: After feeding, your baby should appear content and satisfied.
- Alertness: Your baby should be alert and engaged during their awake periods.
12.2. Signs of Overfeeding
- Frequent Spitting Up: While some spitting up is normal, excessive spitting up after every feeding could indicate overfeeding.
- Excessive Gas: Overfeeding can lead to increased gas and discomfort.
- Loose Stools: Frequent, loose stools can also be a sign of overfeeding.
- Rapid Weight Gain: While weight gain is important, excessively rapid weight gain could be a sign of overfeeding.
12.3. What to Do If You’re Concerned
If you’re concerned that your baby is eating too much or too little, consult with your pediatrician. They can assess your baby’s growth and development and provide personalized recommendations. Avoid restricting your baby’s intake without consulting a healthcare professional.
13. Creating a Feeding Schedule
While responsive feeding is generally recommended, some parents find it helpful to establish a flexible feeding schedule. A schedule can provide structure and predictability, but it’s essential to remain responsive to your baby’s individual needs.
13.1. Sample Feeding Schedule for a 2-Month-Old
Here’s a sample feeding schedule for a 2-month-old, keeping in mind that this is just a guideline and your baby’s actual feeding times may vary:
- 7:00 AM: First feeding of the day
- 10:00 AM: Second feeding
- 1:00 PM: Third feeding
- 4:00 PM: Fourth feeding
- 7:00 PM: Fifth feeding
- 10:00 PM: Sixth feeding
- Night Feedings: As needed (typically 1-2 times per night)
13.2. Tips for Creating a Schedule
- Observe Your Baby: Pay attention to your baby’s natural feeding patterns and try to align the schedule with their needs.
- Be Flexible: Don’t be afraid to adjust the schedule as needed. Growth spurts, illness, or changes in routine can affect your baby’s feeding habits.
- Prioritize Responsive Feeding: Always respond to your baby’s hunger cues, even if it means deviating from the schedule.
- Communicate with Caregivers: If you have other caregivers, such as a partner or nanny, make sure they are aware of the feeding schedule and understand the importance of responsive feeding.
13.3. Benefits of a Flexible Schedule
- Predictability: A schedule can provide a sense of predictability for both you and your baby.
- Routine: It can help establish a routine, which can be beneficial for sleep and overall well-being.
- Peace of Mind: Knowing when to expect feedings can give you peace of mind.
14. Common Questions About Feeding a 2-Month-Old
Here are some frequently asked questions about feeding a 2-month-old baby, along with answers from our experts at HOW.EDU.VN.
14.1. How Often Should a 2-Month-Old Eat?
A 2-month-old typically eats every 2-4 hours, or about 8-12 times in a 24-hour period. Breastfed babies may eat more frequently than formula-fed babies.
14.2. How Much Should a 2-Month-Old Eat at Each Feeding?
A 2-month-old typically eats about 3-4 ounces at each feeding. However, this can vary depending on the baby’s size, appetite, and whether they are breastfed or formula-fed.
14.3. Can I Overfeed My 2-Month-Old?
It’s difficult to overfeed a breastfed baby, as they will naturally stop when they are full. However, it is possible to overfeed a formula-fed baby if you are encouraging them to finish the bottle even when they are showing signs of fullness.
14.4. Is It Normal for My 2-Month-Old to Want to Eat All the Time?
It’s normal for a 2-month-old to go through periods of increased hunger, especially during growth spurts. If your baby seems constantly hungry, offer them more frequent feedings and consult with your pediatrician if you have concerns.
14.5. How Do I Know If My Baby Is Getting Enough to Eat?
Signs that your baby is getting enough to eat include consistent weight gain, adequate diaper output, and contentment after feedings. If you have concerns, consult with your pediatrician.
14.6. What Should I Do If My Baby Is Refusing to Eat?
If your baby is refusing to eat, rule out any medical issues, offer comfort, and try feeding them when they are sleepy. If the refusal to eat persists, consult with your pediatrician or a lactation consultant.
14.7. How Can I Increase My Milk Supply?
If you are breastfeeding and concerned about your milk supply, try nursing more frequently, pumping after feedings, and staying hydrated. Consult with a lactation consultant for personalized advice.
14.8. When Can I Start Introducing Solid Foods?
The American Academy of Pediatrics recommends waiting until around 6 months of age to introduce solid foods. At this age, babies are typically developmentally ready for solids and have a decreased risk of allergies.
14.9. How Do I Transition from Breast Milk to Formula?
If you are transitioning from breast milk to formula, do so gradually to allow your baby’s digestive system to adjust. Start by replacing one breast milk feeding with a formula feeding and gradually increase the number of formula feedings over time.
14.10. Can I Mix Breast Milk and Formula in the Same Bottle?
It’s generally not recommended to mix breast milk and formula in the same bottle, as this can make it difficult to track how much of each your baby is consuming. It’s best to offer breast milk and formula in separate bottles.
15. The Expertise of HOW.EDU.VN: Your Partner in Newborn Care
Understanding your 2-month-old’s feeding needs is a crucial part of providing the best care for your baby. At HOW.EDU.VN, we are committed to providing you with the expert guidance and support you need to navigate the challenges and joys of parenthood. Our team of experienced pediatricians and lactation consultants is here to answer your questions, address your concerns, and help you create a feeding plan that works for you and your baby.
We understand that every baby is unique, and there is no one-size-fits-all approach to feeding. That’s why we offer personalized consultations and tailored advice to meet your individual needs. Whether you are breastfeeding, formula-feeding, or a combination of both, we can provide you with the tools and resources you need to succeed.
16. New Advances in Pediatric Nutrition
Staying current with the latest research and guidelines in pediatric nutrition is essential for providing the best care for your baby. Here are some of the recent advances in the field:
16.1. Human Milk Oligosaccharides (HMOs)
Human Milk Oligosaccharides (HMOs) are complex sugars found naturally in breast milk. Research has shown that HMOs play a crucial role in supporting the development of a healthy gut microbiome and immune system in infants. Some formula manufacturers are now adding HMOs to their formulas to better mimic the benefits of breast milk.
16.2. Probiotics
Probiotics are beneficial bacteria that can help support a healthy gut microbiome. Some studies have shown that probiotics may help reduce the risk of colic, eczema, and other common infant health issues. However, it’s important to talk to your pediatrician before giving your baby probiotics.
16.3. Vitamin D
Vitamin D is essential for bone health and immune function. Breast milk may not provide enough vitamin D, so the American Academy of Pediatrics recommends that all breastfed babies receive a vitamin D supplement. Formula-fed babies also may need a vitamin D supplement if they are not consuming enough formula to meet their vitamin D needs.
16.4. Iron
Iron is essential for healthy brain development. Breast milk is a good source of iron, but breastfed babies may need an iron supplement starting at 4 months of age. Formula-fed babies typically get enough iron from iron-fortified formula.
16.5. Omega-3 Fatty Acids
Omega-3 fatty acids, such as DHA, are important for brain and eye development. Some formula manufacturers are now adding DHA to their formulas. Breastfeeding mothers can also increase their intake of omega-3 fatty acids by eating fatty fish, flaxseeds, and walnuts.
17. New Experts at HOW.EDU.VN
We are excited to announce the addition of several new experts to our team at HOW.EDU.VN. These experienced pediatricians and lactation consultants bring a wealth of knowledge and expertise to our practice.
Table: New Experts at HOW.EDU.VN
| Expert Name | Title | Specialization |
|---|---|---|
| Dr. Emily Carter | Pediatrician | Newborn Nutrition, Growth Spurt Management |
| Dr. Michael Davis | Pediatric Gastroenterologist | Reflux, Colic, Infant Feeding Issues |
| Laura Hernandez, RN | Lactation Consultant | Breastfeeding Support, Milk Supply Issues |
Our new experts are dedicated to providing personalized care and support to families. They are available for consultations and can help you with any questions or concerns you may have about feeding your 2-month-old.
18. Testimonials from Satisfied Parents
Don’t just take our word for it – here’s what some satisfied parents have to say about their experience with HOW.EDU.VN:
“HOW.EDU.VN was a lifesaver when I was struggling with breastfeeding. The lactation consultant helped me with latch issues and gave me the confidence to continue nursing my baby.” – Sarah M.
“I was so worried about whether my baby was getting enough to eat. The pediatrician at HOW.EDU.VN put my mind at ease and gave me a personalized feeding plan that worked perfectly for my baby.” – Jessica L.
“The experts at HOW.EDU.VN are amazing! They are knowledgeable, compassionate, and truly care about helping families. I highly recommend their services.” – Amanda K.
19. Comprehensive Support for Every Stage
At HOW.EDU.VN, we understand that the journey of parenthood is filled with unique challenges and rewards at every stage. From the first few weeks of newborn care to the exciting milestones of toddlerhood and beyond, our team of experts is here to provide you with comprehensive support and guidance every step of the way.
19.1. Newborn Care
The first few months of your baby’s life are a critical time for growth and development. Our newborn care services include:
- Feeding support (breastfeeding and formula-feeding)
- Sleep guidance
- Developmental milestones
- Vaccinations
- Common newborn health issues
19.2. Infant Care
As your baby grows, their needs will change. Our infant care services include:
- Nutrition guidance (introducing solid foods)
- Developmental milestones
- Sleep training
- Safety
- Common infant illnesses
19.3. Toddler Care
Toddlerhood is a time of rapid growth and exploration. Our toddler care services include:
- Nutrition guidance
- Developmental milestones
- Potty training
- Discipline
- Behavioral issues
19.4. Preschool Care
As your child prepares for school, our preschool care services can help them thrive:
- Nutrition guidance
- Developmental milestones
- School readiness
- Social and emotional development
- Common childhood illnesses
19.5. Ongoing Support
We offer ongoing support for families through every stage of parenthood. Our services include:
- Personalized consultations
- Educational resources
- Support groups
- 24/7 access to our online resource library
20. Additional Resources and Support
Navigating the world of newborn feeding can be overwhelming. Remember, you’re not alone. Here are some additional resources to support you:
20.1. Local Support Groups
Connect with other parents in your community through local support groups. Sharing experiences and advice can be invaluable.
20.2. Online Communities
Online forums and social media groups can provide a wealth of information and support. Be sure to vet the sources and seek advice from qualified professionals.
20.3. Books and Websites
Numerous books and websites offer valuable information on newborn feeding and care. Look for resources from reputable organizations and healthcare providers.
20.4. Lactation Consultants
If you’re breastfeeding, a lactation consultant can provide personalized support and guidance.
20.5. Pediatricians
Your pediatrician is your primary resource for all things baby-related. Don’t hesitate to reach out with any questions or concerns.
21. Maximizing Your Baby’s Growth with Expert Feeding Strategies
Optimal nutrition during infancy is crucial for long-term health and development. By implementing expert feeding strategies, you can help your baby achieve their full potential.
21.1. Understanding Nutrient Needs
Infants require a balanced intake of macronutrients (protein, carbohydrates, and fats) and micronutrients (vitamins and minerals) to support their rapid growth and development. Breast milk and formula are designed to provide these essential nutrients.
21.2. Optimizing Breastfeeding
For breastfeeding mothers, optimizing milk production and transfer is key. Frequent nursing, proper latch, and a healthy diet can help ensure your baby gets the nutrients they need.
21.3. Choosing the Right Formula
If you’re formula-feeding, choosing the right formula is essential. Talk to your pediatrician about which type of formula is best for your baby.
21.4. Monitoring Growth and Development
Regular check-ups with your pediatrician are crucial for monitoring your baby’s growth and development. Your pediatrician can assess your baby’s weight, height, and head circumference and provide guidance on feeding and nutrition.
21.5. Addressing Feeding Challenges
If you encounter any feeding challenges, such as refusal to feed or difficulty latching, seek help from a lactation consultant or your pediatrician. Early intervention can help prevent long-term feeding problems.
22. Staying Informed: Pediatric Nutrition Guidelines
Keeping up-to-date with the latest pediatric nutrition guidelines ensures your baby receives the best possible care.
22.1. American Academy of Pediatrics (AAP)
The AAP is a leading authority on child health and nutrition. Their website offers a wealth of information on newborn feeding and care.
22.2. World Health Organization (WHO)
The WHO provides global recommendations on infant and young child feeding. Their guidelines emphasize the importance of breastfeeding for the first six months of life.
22.3. Centers for Disease Control and Prevention (CDC)
The CDC offers valuable information on infant nutrition and health. Their website includes resources on breastfeeding, formula-feeding, and introducing solid foods.
22.4. Registered Dietitian Nutritionists (RDNs)
RDNs are nutrition experts who can provide personalized guidance on infant feeding and nutrition. Consult with an RDN for tailored advice.
22.5. Staying Current
Stay informed about the latest pediatric nutrition guidelines by subscribing to reputable newsletters, attending conferences, and reading peer-reviewed journals.
23. Connecting with Experts at HOW.EDU.VN
Are you looking for expert advice on how much your 2-month-old should eat or dealing with feeding challenges? At HOW.EDU.VN, our team of experienced pediatricians and lactation consultants is here to provide personalized guidance and support.
23.1. Personalized Consultations
We offer personalized consultations to address your specific concerns and develop a feeding plan that works for you and your baby.
23.2. Expert Advice
Our team of experts stays up-to-date on the latest pediatric nutrition guidelines and can provide you with evidence-based recommendations.
23.3. Support and Encouragement
We understand that parenthood can be challenging, and we are here to provide you with the support and encouragement you need to succeed.
23.4. Access to Resources
We offer access to a wealth of resources, including educational materials, support groups, and online forums.
23.5. Convenient and Affordable
Our services are convenient and affordable, making it easy to get the help you need.
24. Frequently Asked Questions (FAQs) About Infant Feeding
Here are some frequently asked questions about infant feeding, answered by our experts at HOW.EDU.VN.
24.1. How Much Formula Should a 2-Month-Old Drink?
A 2-month-old typically drinks about 3-4 ounces of formula per feeding, or about 24-32 ounces in a 24-hour period.
24.2. Can I Give My 2-Month-Old Water?
No, you should not give your 2-month-old water. Breast milk or formula provides all the fluids your baby needs.
24.3. How Do I Know If My Baby Is Allergic to Formula?
Signs of a formula allergy include rash, vomiting, diarrhea, and fussiness. If you suspect your baby is allergic to formula, talk to your pediatrician.
24.4. What Is the Best Way to Warm a Bottle?
The best way to warm a bottle is to place it in a bowl of warm water for a few minutes. Avoid using a microwave, as this can create hot spots.
24.5. How Long Is Formula Good For After Mixing?
Prepared formula should be used within 1 hour of mixing and any leftover formula should be discarded.
24.6. Can I Freeze Breast Milk?
Yes, you can freeze breast milk. Breast milk can be stored in the freezer for up to 6 months.
24.7. How Do I Thaw Breast Milk?
The best way to thaw breast milk is to place it in the refrigerator overnight. You can also thaw it by placing it in a bowl of warm water.
24.8. How Long Is Breast Milk Good For After Thawing?
Thawed breast milk should be used within 24 hours.
24.9. What Should I Do If My Baby Has Gas?
To help relieve gas, burp your baby frequently, try bicycle exercises, and consider using gas drops.
24.10. When Should I Start Giving My Baby a Pacifier?
You can start giving your baby a pacifier as soon as breastfeeding is well-established, typically around 3-4 weeks of age.
25. Conclusion: Partnering for Your Baby’s Best Start
Understanding how much your 2-month-old should eat is an essential part of ensuring their healthy growth and development. By paying attention to your baby’s cues, seeking expert advice when needed, and staying informed about the latest guidelines, you can provide your little one with the best possible start in life.
Remember, every baby is unique, and what works for one family may not work for another. Trust your instincts, be patient, and don’t hesitate to reach out for support when you need it. At HOW.EDU.VN, we are here to partner with you on this incredible journey.
Want personalized advice on your baby’s feeding needs? Contact our expert pediatricians and lactation consultants at HOW.EDU.VN today.
Address: 456 Expertise Plaza, Consult City, CA 90210, United States
WhatsApp: +1 (310) 555-1212
Website: how.edu.vn
Our team is ready to help you navigate the joys and challenges of newborn care.