How Much Urine Can The Bladder Hold? Understanding your bladder’s capacity is crucial for maintaining urinary health and overall well-being. At HOW.EDU.VN, our team of expert doctors can provide personalized advice to help you optimize your bladder function. Learn about bladder capacity, factors affecting it, and when to seek professional consultation for bladder-related issues.
1. Understanding Bladder Capacity: An Overview
The bladder, a crucial organ in the urinary system, functions as a reservoir for urine produced by the kidneys. Understanding its capacity is essential for grasping how frequently one needs to urinate and recognizing potential bladder-related issues. A typical adult bladder can hold approximately 500 milliliters (mL) or about 2 cups of urine comfortably. However, the sensation to urinate usually arises when the bladder contains around 150 to 200 mL. This early urge serves as a gentle reminder, allowing individuals to plan a bathroom visit without experiencing urgency or discomfort.
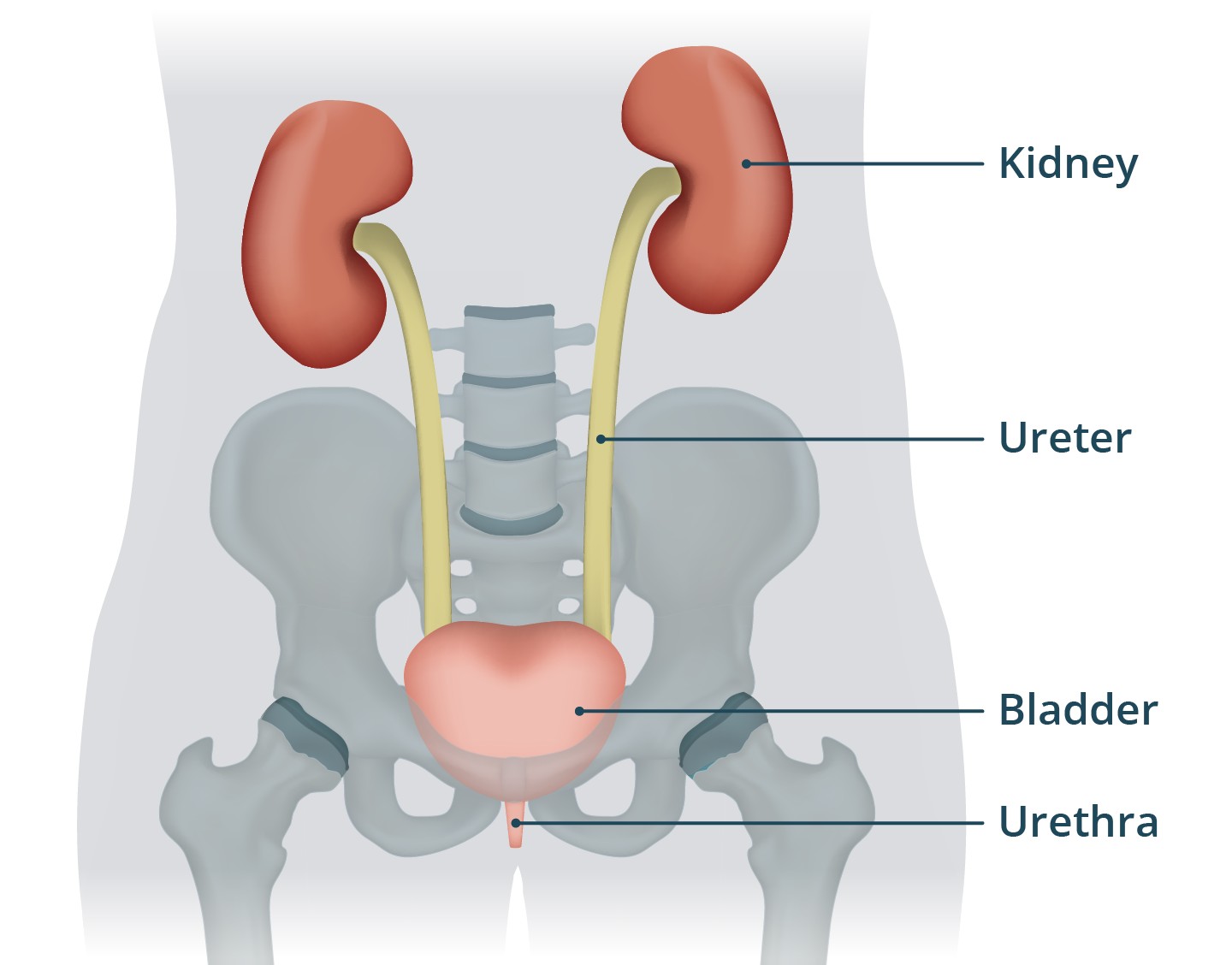 Diagram of a healthy bladder filling with urine.
Diagram of a healthy bladder filling with urine.
The bladder’s ability to stretch and contract is due to its unique composition of smooth muscle fibers known as the detrusor muscle. As urine accumulates, the bladder expands, and nerve endings in the bladder wall send signals to the brain, indicating the level of fullness. The brain then signals back to the bladder and urinary sphincters to control the release of urine. This intricate communication between the bladder and the brain allows for voluntary control over urination, enabling individuals to postpone voiding until a convenient time and location. Understanding this mechanism is the first step in appreciating the complexities of bladder function.
2. Factors Influencing Bladder Capacity
Several factors can affect how much urine the bladder can hold. These include age, sex, hydration levels, and certain medical conditions.
2.1. Age-Related Changes
As we age, the bladder’s capacity tends to decrease. This is due to changes in the elasticity of the bladder muscles and a decrease in the ability to postpone urination. Older adults may experience a more frequent urge to urinate, especially at night (nocturia). Additionally, the bladder muscles may weaken, leading to incomplete emptying and an increased risk of urinary tract infections (UTIs). These age-related changes are a natural part of the aging process and can be managed through lifestyle adjustments, bladder training exercises, and, if necessary, medical interventions. At HOW.EDU.VN, our geriatric health specialists can provide tailored advice to manage age-related bladder issues effectively.
2.2. Gender Differences
There are slight differences in bladder capacity between males and females. Generally, males tend to have a slightly larger bladder capacity due to anatomical differences. Additionally, hormonal changes during menstruation, pregnancy, and menopause can affect bladder function in females. Pregnancy, in particular, can significantly impact bladder capacity due to the growing uterus pressing against the bladder, leading to increased urinary frequency and urgency. Understanding these gender-specific factors is crucial for tailoring treatment approaches and providing targeted care.
2.3. Hydration Levels
The amount of fluid you consume directly affects how often you need to urinate. High fluid intake leads to increased urine production, filling the bladder more quickly. Conversely, dehydration can reduce urine production, but it can also irritate the bladder. It’s essential to maintain a balanced fluid intake to support healthy bladder function. The color of your urine can be a simple indicator of your hydration status; pale yellow urine usually indicates adequate hydration, while dark yellow or amber urine suggests dehydration. Consulting with our nutrition experts at HOW.EDU.VN can help you establish optimal hydration habits for bladder health.
2.4. Medical Conditions
Certain medical conditions can significantly affect bladder capacity and function. These include:
-
Diabetes: High blood sugar levels can lead to increased urine production and bladder irritation.
-
Urinary Tract Infections (UTIs): Infections can cause inflammation and reduce bladder capacity.
-
Overactive Bladder (OAB): This condition causes frequent and urgent urination due to involuntary bladder muscle contractions.
-
Interstitial Cystitis: Also known as painful bladder syndrome, this chronic condition causes bladder pain and frequent urination.
-
Neurological Disorders: Conditions like multiple sclerosis, Parkinson’s disease, and stroke can affect the nerves controlling bladder function, leading to incontinence or urinary retention.
Managing these conditions often requires a comprehensive approach, including medication, lifestyle modifications, and specialized therapies. At HOW.EDU.VN, our multidisciplinary team of specialists can provide integrated care to address the underlying causes of bladder dysfunction and improve your quality of life.
3. What Happens When You Hold Your Urine Too Long?
While the bladder is designed to hold urine, repeatedly delaying urination can lead to several adverse effects.
3.1. Bladder Stretching
Consistently holding urine can stretch the bladder muscles beyond their normal capacity. Over time, this can weaken the bladder muscles, making it harder to empty the bladder completely. Incomplete bladder emptying can lead to urinary stasis, increasing the risk of bacterial growth and UTIs. Additionally, chronic bladder stretching can desensitize the nerves that signal bladder fullness, leading to reduced awareness of the need to urinate.
3.2. Increased Risk of UTIs
Holding urine for extended periods allows bacteria to multiply in the bladder, increasing the risk of urinary tract infections. Bacteria that normally get flushed out during urination can proliferate, leading to infection and inflammation. Symptoms of a UTI include frequent urination, painful urination (dysuria), a burning sensation, and cloudy or bloody urine. Prompt treatment with antibiotics is usually necessary to resolve the infection and prevent complications.
3.3. Bladder Pain and Discomfort
When the bladder becomes overly full, it can cause pain and discomfort in the lower abdomen and pelvic area. This discomfort can range from a mild ache to sharp, intense pain. Additionally, holding urine can lead to muscle spasms in the bladder and pelvic floor, exacerbating the pain. Frequent episodes of bladder pain can significantly impact daily activities and overall quality of life.
3.4. Kidney Problems
In rare cases, repeatedly holding urine can lead to kidney problems. When the bladder is full, urine can back up into the kidneys, causing hydronephrosis (swelling of the kidneys). This can damage the kidneys and impair their ability to filter waste products from the blood. Chronic hydronephrosis can lead to kidney failure and other serious complications. Although rare, it’s essential to avoid repeatedly holding urine to protect kidney health.
4. How to Improve Your Bladder Capacity
While you can’t significantly increase the size of your bladder, you can train it to hold more urine comfortably and reduce the frequency of urination.
4.1. Bladder Training
Bladder training involves gradually increasing the intervals between trips to the bathroom. Start by delaying urination for a few minutes each time you feel the urge, gradually increasing the delay over several weeks. This helps stretch the bladder and improve your control over the urge to urinate. Bladder training also involves keeping a bladder diary to track your urination habits and identify patterns.
4.2. Pelvic Floor Exercises (Kegels)
Strengthening your pelvic floor muscles can improve bladder control and reduce urinary urgency and frequency. Kegel exercises involve contracting and relaxing the pelvic floor muscles, which support the bladder and urethra. To perform Kegels, squeeze the muscles as if you’re stopping the flow of urine, hold for a few seconds, and then relax. Repeat this exercise several times a day.
4.3. Fluid Management
Adjusting your fluid intake can help manage bladder symptoms. Avoid drinking large amounts of fluid at once and limit your intake of caffeine and alcohol, which can irritate the bladder. It’s also helpful to avoid drinking fluids close to bedtime to reduce nighttime urination. Distribute your fluid intake evenly throughout the day to maintain adequate hydration without overloading the bladder.
4.4. Diet Modifications
Certain foods and beverages can irritate the bladder and worsen urinary symptoms. Common bladder irritants include caffeine, alcohol, carbonated drinks, artificial sweeteners, spicy foods, and acidic fruits like citrus. Identifying and eliminating these triggers from your diet can help reduce bladder irritation and improve bladder control. Keeping a food diary can help you identify specific foods that exacerbate your symptoms.
5. When to Seek Medical Advice
It’s essential to seek medical advice if you experience any of the following symptoms:
- Frequent urinary tract infections
- Blood in your urine
- Painful urination
- Difficulty emptying your bladder
- Urinary incontinence
- Sudden changes in bladder habits
These symptoms could indicate an underlying medical condition that requires diagnosis and treatment. Consulting with a healthcare professional can help identify the cause of your symptoms and develop an appropriate management plan. At HOW.EDU.VN, our expert doctors are available to provide comprehensive evaluations and personalized treatment recommendations.
6. Expert Insights from HOW.EDU.VN Doctors
At HOW.EDU.VN, we pride ourselves on having a team of over 100 renowned doctors with extensive experience in urology and related fields. Our experts offer personalized advice and treatment plans to address your specific bladder concerns.
6.1. Dr. Emily Carter, Urologist
“Maintaining optimal bladder health involves a combination of lifestyle adjustments, bladder training, and, when necessary, medical interventions. It’s crucial to listen to your body and seek professional help if you experience persistent bladder issues,” says Dr. Carter.
6.2. Dr. David Lee, Geriatric Specialist
“Age-related changes in bladder function are common, but they don’t have to diminish your quality of life. With the right strategies and support, older adults can effectively manage bladder symptoms and maintain their independence,” advises Dr. Lee.
6.3. Dr. Sarah Johnson, Nutritionist
“Diet plays a significant role in bladder health. Identifying and avoiding bladder irritants can make a noticeable difference in reducing urinary symptoms. A balanced diet and adequate hydration are key to supporting overall bladder function,” explains Dr. Johnson.
7. Addressing Common Misconceptions About Bladder Capacity
Several misconceptions exist regarding bladder capacity and function. Let’s address some of the most common ones:
7.1. Myth: Holding Your Urine Strengthens Your Bladder
Fact: Repeatedly holding urine can weaken the bladder muscles and increase the risk of UTIs. It’s essential to empty your bladder regularly to maintain optimal bladder health.
7.2. Myth: Drinking Less Water Will Reduce Urinary Frequency
Fact: Restricting fluid intake can lead to dehydration and bladder irritation. It’s important to drink enough water to maintain adequate hydration and support overall health.
7.3. Myth: Urinary Incontinence Is a Normal Part of Aging
Fact: While age-related changes can affect bladder function, urinary incontinence is not a normal part of aging. It can be effectively managed with appropriate treatment and lifestyle adjustments.
7.4. Myth: Bladder Problems Are Only a Concern for Older Adults
Fact: Bladder problems can affect people of all ages. Conditions like UTIs, overactive bladder, and interstitial cystitis can occur in younger individuals as well.
8. The Role of Technology in Monitoring Bladder Health
Advancements in technology have led to innovative tools for monitoring bladder health. Wearable sensors and smartphone apps can track urination patterns, fluid intake, and other relevant data, providing valuable insights for individuals and healthcare professionals. These technologies can help identify trends, monitor treatment effectiveness, and improve overall bladder management.
9. Case Studies: Success Stories from HOW.EDU.VN
9.1. Case Study 1: Managing Overactive Bladder
A 45-year-old female presented with symptoms of overactive bladder, including frequent urination and urgency. After a comprehensive evaluation at HOW.EDU.VN, she was started on bladder training, pelvic floor exercises, and dietary modifications. Within a few weeks, her symptoms significantly improved, and she was able to regain control over her bladder function.
9.2. Case Study 2: Treating Recurrent UTIs
A 60-year-old male had a history of recurrent UTIs. At HOW.EDU.VN, he underwent a thorough evaluation to identify underlying risk factors. He was prescribed prophylactic antibiotics, along with lifestyle recommendations to prevent future infections. As a result, he experienced a significant reduction in the frequency of UTIs.
9.3. Case Study 3: Addressing Urinary Incontinence After Pregnancy
A 32-year-old female developed urinary incontinence after childbirth. She received pelvic floor therapy and bladder training at HOW.EDU.VN. Within a few months, she was able to regain full bladder control and improve her quality of life.
10. Understanding the Science Behind Bladder Function
The bladder is a complex organ with intricate physiological mechanisms that govern its function. Understanding the science behind bladder function can help individuals appreciate the importance of maintaining bladder health.
10.1. The Micturition Reflex
The micturition reflex is the process by which the bladder empties urine. It involves a coordinated interaction between the bladder muscles, nerves, and brain. As the bladder fills with urine, stretch receptors in the bladder wall send signals to the brain, indicating the level of fullness. The brain then signals back to the bladder and urinary sphincters to control the release of urine. Voluntary control over urination is achieved through conscious regulation of this reflex.
10.2. The Role of the Detrusor Muscle
The detrusor muscle is the smooth muscle layer of the bladder wall. It contracts to expel urine during urination. The detrusor muscle is controlled by the autonomic nervous system, which regulates involuntary functions like bladder contraction. In conditions like overactive bladder, the detrusor muscle contracts involuntarily, leading to urinary urgency and frequency.
10.3. The Urinary Sphincters
The urinary sphincters are muscles that control the flow of urine from the bladder. The internal sphincter is located at the junction of the bladder and urethra, while the external sphincter is located further down the urethra. These sphincters work together to maintain urinary continence and prevent leakage.
11. Practical Tips for Maintaining Bladder Health
- Empty your bladder regularly: Avoid holding urine for extended periods.
- Stay hydrated: Drink enough water to maintain adequate hydration.
- Avoid bladder irritants: Limit your intake of caffeine, alcohol, and acidic foods.
- Practice pelvic floor exercises: Strengthen your pelvic floor muscles to improve bladder control.
- Maintain a healthy weight: Obesity can increase pressure on the bladder and worsen urinary symptoms.
- Quit smoking: Smoking can irritate the bladder and increase the risk of bladder cancer.
- Manage underlying medical conditions: Control diabetes, UTIs, and other conditions that can affect bladder function.
12. Future Directions in Bladder Research
Ongoing research is focused on developing new and improved treatments for bladder disorders. Areas of interest include:
- Novel medications: Developing drugs that target specific pathways involved in bladder dysfunction.
- Advanced neuromodulation techniques: Using electrical stimulation to modulate nerve activity and improve bladder control.
- Gene therapy: Targeting specific genes to correct bladder dysfunction.
- Regenerative medicine: Using stem cells and tissue engineering to regenerate damaged bladder tissue.
13. How HOW.EDU.VN Can Help You
At HOW.EDU.VN, we understand the impact that bladder problems can have on your quality of life. Our team of expert doctors offers comprehensive evaluations, personalized treatment plans, and ongoing support to help you regain control over your bladder function.
13.1. Personalized Consultations
Our doctors take the time to listen to your concerns, understand your symptoms, and develop a tailored treatment plan that meets your individual needs. We offer both in-person and virtual consultations for your convenience.
13.2. Comprehensive Evaluations
We use state-of-the-art diagnostic tools to accurately assess your bladder function and identify any underlying medical conditions. Our evaluations include urodynamic testing, cystoscopy, and imaging studies.
13.3. Multidisciplinary Approach
Our team includes urologists, geriatric specialists, nutritionists, and other healthcare professionals who work together to provide integrated care. We address all aspects of your bladder health, from medical management to lifestyle adjustments.
13.4. Ongoing Support
We provide ongoing support and education to help you manage your bladder symptoms and maintain your overall well-being. Our resources include educational materials, support groups, and online forums.
14. Conclusion: Taking Control of Your Bladder Health
Understanding how much urine the bladder can hold, the factors that influence its capacity, and the steps you can take to maintain bladder health is crucial for overall well-being. At HOW.EDU.VN, our team of expert doctors is dedicated to providing personalized care and support to help you regain control over your bladder function. Don’t let bladder problems diminish your quality of life. Contact us today to schedule a consultation and take the first step towards better bladder health.
15. FAQs About Bladder Capacity
15.1. How Much Urine Can the Bladder Hold on Average?
The average adult bladder can hold about 500 mL (2 cups) of urine. The urge to urinate typically occurs when the bladder is about one-third full.
15.2. Is It Bad to Hold Your Urine Regularly?
Yes, regularly holding urine can weaken the bladder muscles and increase the risk of urinary tract infections.
15.3. Can You Increase Your Bladder Capacity?
While you can’t significantly increase the size of your bladder, you can train it to hold more urine comfortably through bladder training exercises.
15.4. What Are the Symptoms of an Overactive Bladder?
Symptoms of overactive bladder include frequent urination, urinary urgency, and urge incontinence.
15.5. How Can You Strengthen Your Bladder Muscles?
You can strengthen your bladder muscles by performing pelvic floor exercises (Kegels) regularly.
15.6. What Foods and Drinks Irritate the Bladder?
Common bladder irritants include caffeine, alcohol, carbonated drinks, artificial sweeteners, spicy foods, and acidic fruits.
15.7. When Should You See a Doctor for Bladder Problems?
You should see a doctor if you experience frequent UTIs, blood in your urine, painful urination, difficulty emptying your bladder, or urinary incontinence.
15.8. How Is Urinary Incontinence Treated?
Urinary incontinence can be treated with lifestyle adjustments, bladder training, pelvic floor exercises, medications, and surgery.
15.9. Can Diabetes Affect Bladder Function?
Yes, diabetes can lead to increased urine production and bladder irritation due to high blood sugar levels.
15.10. What Is the Role of Hydration in Bladder Health?
Adequate hydration is essential for bladder health. Drinking enough water helps maintain optimal bladder function and prevents dehydration.
Are you struggling with bladder issues and seeking expert advice? Connect with our team of over 100 renowned doctors at HOW.EDU.VN for personalized consultations and comprehensive treatment plans. We understand the challenges you face and are dedicated to helping you regain control over your bladder health.
Contact us today:
- Address: 456 Expertise Plaza, Consult City, CA 90210, United States
- WhatsApp: +1 (310) 555-1212
- Website: HOW.EDU.VN
Let how.edu.vn be your trusted partner in achieving optimal bladder health and overall well-being. Our experts are here to provide the guidance and support you need to live your life to the fullest.