At HOW.EDU.VN, we understand your curiosity about bladder capacity and urinary health. Understanding How Much A Bladder Can Hold is crucial for managing urinary frequency, incontinence, and overall bladder health. Learn more about typical bladder volumes, factors affecting capacity, and expert advice for maintaining a healthy urinary system. For personalized guidance and expert solutions, consult our team of over 100 renowned PhDs.
1. Understanding Bladder Capacity
The urinary bladder is a muscular, balloon-like organ that stores urine before it is eliminated from the body. Its ability to stretch and hold varying amounts of fluid is essential for maintaining continence and allowing individuals to urinate at convenient times. But what exactly determines bladder volume and what is considered normal?
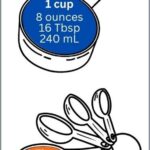
1.1 Average Bladder Capacity in Adults
On average, a healthy adult bladder can hold between 300 to 500 milliliters (ml), which is roughly 10 to 17 ounces. However, this capacity can vary based on several factors, including age, gender, and individual physiology.
1.2 Gender Differences in Bladder Size
Generally, men tend to have slightly larger bladder capacities than women. While women can typically hold up to 500 ml, men can often store up to 700 ml of urine. This difference is often attributed to anatomical variations and muscle mass.
1.3 Initial Urge vs. Full Bladder
Most people begin to feel the initial urge to urinate when the bladder contains about 150 to 250 ml of urine. This sensation is a signal from the nerves in the bladder wall to the brain, indicating that it’s time to start thinking about finding a restroom. However, a healthy bladder can comfortably hold more urine before reaching its maximum capacity.
2. Factors Affecting Bladder Capacity
Several factors can influence bladder storage volume and the frequency of urination. Understanding these factors is key to addressing and managing bladder-related issues effectively.
2.1 Age-Related Changes
As people age, the bladder’s elasticity and capacity may decrease. This can lead to more frequent urination and an increased risk of urinary incontinence. Age-related conditions like an enlarged prostate in men can also affect bladder function.
2.2 Medical Conditions and Medications
Various medical conditions, such as diabetes, urinary tract infections (UTIs), and overactive bladder (OAB), can impact bladder capacity. Medications like diuretics can also increase urine production, leading to a fuller bladder more often.
2.3 Lifestyle Habits: Fluid Intake and Diet
Fluid intake plays a significant role in bladder volume. Consuming large amounts of liquids, especially caffeinated or alcoholic beverages, can increase urine production and the need to urinate more frequently. Certain acidic foods and drinks can also irritate the bladder, reducing its functional capacity.
2.4 Muscle Tone and Pelvic Floor Health
The strength of the pelvic floor muscles is crucial for bladder control. Weak pelvic floor muscles can reduce bladder capacity and increase the likelihood of urinary leakage. Regular pelvic floor exercises, like Kegels, can help improve muscle tone and bladder control.
Alt: Anatomical illustration showing the location of kidneys and bladder in the human body, highlighting urinary system
3. Medical Conditions Affecting Bladder Capacity
Several medical conditions can significantly impact bladder capacity and function. Identifying and managing these conditions is crucial for maintaining urinary health.
3.1 Overactive Bladder (OAB)
Overactive bladder (OAB) is a condition characterized by a sudden, uncontrollable urge to urinate. This urge can occur frequently throughout the day and night, reducing the effective bladder capacity. OAB can result from nerve damage, muscle dysfunction, or other underlying health issues.
3.2 Urinary Tract Infections (UTIs)
Urinary tract infections (UTIs) are infections that affect the bladder, urethra, or kidneys. UTIs can cause inflammation and irritation of the bladder lining, leading to a reduced bladder capacity and frequent, painful urination.
3.3 Interstitial Cystitis (IC)
Interstitial cystitis (IC), also known as painful bladder syndrome, is a chronic condition that causes bladder pain and frequent urination. IC can lead to a decreased bladder capacity and a persistent urge to urinate, even when the bladder is not full.
3.4 Benign Prostatic Hyperplasia (BPH)
In men, benign prostatic hyperplasia (BPH), or an enlarged prostate, can compress the urethra and obstruct urine flow. This obstruction can lead to incomplete bladder emptying, increased urinary frequency, and a reduced functional bladder capacity.
4. Symptoms of Bladder Capacity Issues
Recognizing the symptoms of bladder control problems is the first step toward seeking appropriate medical advice and treatment.
4.1 Frequent Urination (Frequency)
Frequent urination, or frequency, is defined as needing to urinate more than eight times in a 24-hour period. This can be a sign of reduced bladder capacity or an underlying condition affecting bladder function.
4.2 Urgent Need to Urinate (Urgency)
Urgency is a sudden, strong urge to urinate that is difficult to control. This symptom is often associated with overactive bladder (OAB) and can significantly impact daily activities.
4.3 Nocturia (Nighttime Urination)
Nocturia is the need to wake up multiple times during the night to urinate. This symptom can disrupt sleep patterns and may indicate a bladder capacity issue or other medical condition.
4.4 Urinary Incontinence (Leakage)
Urinary incontinence is the involuntary leakage of urine. This can occur due to weakened pelvic floor muscles, overactive bladder, or other factors affecting bladder control. There are several types of urinary incontinence, including stress incontinence (leakage with physical activity), urge incontinence (leakage associated with urgency), and overflow incontinence (leakage due to incomplete bladder emptying).
5. Diagnosing Bladder Capacity Issues
If you are experiencing symptoms of reduced bladder capacity or other urinary problems, it’s essential to consult with a healthcare professional for proper diagnosis and treatment.
5.1 Medical History and Physical Exam
Your doctor will begin by taking a detailed medical history, asking about your symptoms, fluid intake, medications, and any underlying health conditions. A physical exam may also be performed to assess your overall health and identify any potential causes of your bladder issues.
5.2 Bladder Diary and Urinalysis
Keeping a bladder diary, where you record your fluid intake, urination frequency, and any episodes of leakage, can provide valuable information about your bladder function. A urinalysis, which involves testing a sample of your urine, can help detect infections, blood, or other abnormalities.
5.3 Urodynamic Testing
Urodynamic testing is a series of tests that assess how well your bladder, sphincters, and urethra are storing and releasing urine. These tests can help identify the cause of your bladder problems and guide treatment decisions. Common urodynamic tests include cystometry (measuring bladder pressure), uroflowmetry (measuring urine flow rate), and post-void residual measurement (measuring the amount of urine left in your bladder after urination).
5.4 Cystoscopy
Cystoscopy is a procedure in which a thin, flexible tube with a camera (cystoscope) is inserted into your urethra to visualize the inside of your bladder. This procedure can help identify abnormalities such as tumors, stones, or inflammation.
6. Managing and Improving Bladder Capacity
There are several strategies you can employ to manage and potentially improve your bladder control. These methods range from lifestyle modifications to medical interventions.
6.1 Bladder Training Techniques
Bladder training involves gradually increasing the time between trips to the bathroom. This technique can help improve bladder capacity and reduce urgency and frequency.
Step-by-Step Guide to Bladder Training:
- Keep a Bladder Diary: Record the times you urinate and any episodes of urgency or leakage.
- Set a Schedule: Start by urinating at fixed intervals, such as every hour.
- Gradually Increase Intervals: Once you are comfortable, gradually increase the time between trips to the bathroom by 15-30 minutes each week.
- Practice Urgency Control: When you feel the urge to urinate before your scheduled time, try to delay urination by using techniques such as deep breathing or distraction.
- Stay Consistent: Continue to follow your bladder training schedule, even when you don’t feel the urge to urinate.
6.2 Pelvic Floor Exercises (Kegels)
Pelvic floor exercises, also known as Kegels, involve repeatedly contracting and relaxing the muscles that support the bladder, uterus, and rectum. Strengthening these muscles can improve bladder control and reduce urinary leakage.
How to Perform Kegel Exercises:
- Identify the Right Muscles: To identify your pelvic floor muscles, try stopping your urine flow midstream. The muscles you use to do this are your pelvic floor muscles.
- Contract and Relax: Squeeze your pelvic floor muscles for 5 seconds, then relax for 5 seconds.
- Repeat: Repeat this exercise 10-15 times, three times a day.
- Consistency is Key: Perform Kegel exercises regularly for several weeks to see noticeable improvements.
6.3 Dietary Adjustments
Making changes to your diet can help reduce bladder irritation and improve bladder capacity.
Dietary Tips for Bladder Health:
- Limit Caffeine and Alcohol: These substances can irritate the bladder and increase urine production.
- Avoid Acidic Foods: Citrus fruits, tomatoes, and spicy foods can worsen bladder symptoms.
- Stay Hydrated: Drink plenty of water throughout the day, but avoid drinking large amounts of fluids before bedtime.
- Monitor Your Diet: Keep a food diary to identify any specific foods that may be triggering your bladder symptoms.
6.4 Medications and Medical Treatments
In some cases, medications or medical treatments may be necessary to manage bladder capacity issues. Medications such as anticholinergics can help reduce bladder spasms and urgency, while other treatments like Botox injections or nerve stimulation may be used to improve bladder control.
7. The Role of Experts in Managing Bladder Health
When dealing with persistent or severe bladder capacity issues, seeking advice from experts is crucial. At HOW.EDU.VN, our team of over 100 PhDs offers specialized guidance to help you regain control over your bladder health.
7.1 Benefits of Consulting with Specialists at HOW.EDU.VN
Consulting with our experts provides several key advantages:
- Personalized Assessment: Our specialists conduct thorough assessments to understand your unique situation and needs.
- Tailored Treatment Plans: We develop customized treatment plans based on the latest scientific evidence and clinical best practices.
- Advanced Diagnostic Techniques: We utilize advanced diagnostic techniques to accurately identify the underlying causes of your bladder problems.
- Comprehensive Support: Our team provides ongoing support and education to help you manage your bladder health effectively.
7.2 Areas of Expertise
Our experts at HOW.EDU.VN specialize in various areas related to bladder health, including:
| Area of Expertise | Description |
|---|---|
| Urology | Diagnosis and treatment of disorders of the urinary tract and male reproductive organs. |
| Gynecology | Diagnosis and treatment of conditions affecting the female reproductive system and urinary tract. |
| Geriatrics | Management of age-related bladder issues and urinary incontinence in older adults. |
| Physical Therapy | Pelvic floor muscle rehabilitation and bladder training techniques. |
| Neurology | Management of bladder problems related to neurological conditions such as multiple sclerosis or Parkinson’s disease. |
8. Innovative Approaches to Bladder Capacity Management
Advancements in medical technology and research have led to innovative approaches for managing bladder control and capacity.
8.1 Neuromodulation Techniques
Neuromodulation techniques, such as sacral nerve stimulation (SNS) and percutaneous tibial nerve stimulation (PTNS), involve stimulating nerves to improve bladder function. These treatments can help reduce urgency, frequency, and urinary incontinence.
8.2 Minimally Invasive Surgical Options
For individuals with severe bladder problems, minimally invasive surgical options may be considered. These procedures can help improve bladder capacity and reduce urinary leakage. Examples include bladder augmentation (increasing bladder size) and sling surgery (supporting the urethra).
8.3 Advanced Pharmacological Interventions
New medications are continually being developed to target specific bladder problems. These advanced pharmacological interventions can help improve bladder capacity and reduce the symptoms of overactive bladder and other urinary conditions.
9. Success Stories: How HOW.EDU.VN Experts Have Helped
Real-life examples illustrate the effectiveness of expert guidance in managing bladder health. Here are a few success stories from HOW.EDU.VN:
9.1 Case Study 1: Overactive Bladder
Sarah, a 45-year-old woman, struggled with overactive bladder (OAB) for several years. She experienced frequent urination, urgency, and nighttime urination, which significantly impacted her quality of life. After consulting with a specialist at HOW.EDU.VN, Sarah underwent a comprehensive assessment and was prescribed a tailored treatment plan that included bladder training, pelvic floor exercises, and medication. Within a few months, Sarah experienced a significant reduction in her OAB symptoms and regained control over her bladder function.
9.2 Case Study 2: Stress Incontinence
John, a 60-year-old man, developed stress incontinence after prostate surgery. He experienced urinary leakage during physical activities such as running and lifting weights. John sought help from a physical therapist at HOW.EDU.VN who specialized in pelvic floor rehabilitation. Through targeted exercises and biofeedback techniques, John was able to strengthen his pelvic floor muscles and significantly reduce his stress incontinence.
9.3 Case Study 3: Interstitial Cystitis
Emily, a 35-year-old woman, was diagnosed with interstitial cystitis (IC), a chronic condition causing bladder pain and frequent urination. She consulted with a urologist at HOW.EDU.VN who specialized in IC management. Emily received a comprehensive treatment plan that included dietary modifications, bladder instillations, and pain management strategies. Over time, Emily experienced a significant reduction in her bladder pain and improved her overall quality of life.
10. Preventive Measures for Maintaining Healthy Bladder Capacity
Taking proactive steps can help maintain a healthy bladder capacity and prevent urinary problems.
10.1 Regular Exercise and a Healthy Lifestyle
Regular physical activity can help maintain a healthy weight and improve overall health, including bladder function. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
10.2 Proper Hydration Habits
Drinking adequate amounts of water is essential for maintaining bladder health. However, it’s important to avoid drinking excessive amounts of fluids, especially before bedtime.
10.3 Pelvic Floor Muscle Strengthening
Performing Kegel exercises regularly can help strengthen the pelvic floor muscles and improve bladder control. Make Kegels a part of your daily routine to support long-term bladder health.
10.4 Avoiding Bladder Irritants
Limiting your intake of caffeine, alcohol, acidic foods, and other bladder irritants can help reduce bladder symptoms and improve bladder capacity.
11. Addressing Common Myths About Bladder Capacity
It’s important to dispel common misconceptions about bladder capacity to ensure informed decision-making regarding your health.
11.1 Myth: Holding Urine Can Stretch Your Bladder
While the bladder is a flexible organ, repeatedly holding urine for extended periods can weaken the bladder muscles over time, potentially leading to urinary retention or incontinence.
11.2 Myth: Drinking Less Water Will Improve Bladder Control
Dehydration can actually worsen bladder symptoms by concentrating urine, which can irritate the bladder lining and increase urgency. It’s important to stay properly hydrated to maintain bladder health.
11.3 Myth: Urinary Incontinence is a Normal Part of Aging
While age-related changes can affect bladder function, urinary incontinence is not a normal part of aging. It is a treatable condition, and seeking medical help can significantly improve quality of life.
11.4 Myth: Only Women Experience Bladder Control Problems
Both men and women can experience bladder control problems. Conditions such as benign prostatic hyperplasia (BPH) in men can lead to urinary frequency, urgency, and incontinence.
12. The Future of Bladder Health Management
Ongoing research and technological advancements are paving the way for innovative solutions in bladder health management.
12.1 Advancements in Diagnostic Tools
New diagnostic tools are being developed to provide more accurate and detailed assessments of bladder function. These advancements can help healthcare professionals diagnose bladder problems earlier and develop more effective treatment plans.
12.2 Personalized Treatment Approaches
Personalized medicine is becoming increasingly important in bladder health management. By considering individual factors such as genetics, lifestyle, and medical history, healthcare providers can develop treatment plans that are tailored to each patient’s specific needs.
12.3 Telehealth and Remote Monitoring
Telehealth and remote monitoring technologies are making it easier for individuals to access expert care and monitor their bladder health from the comfort of their homes. These technologies can improve patient engagement and adherence to treatment plans.
13. Seeking Expert Advice at HOW.EDU.VN: A Comprehensive Guide
Navigating bladder health issues can be complex, but with the right guidance, you can achieve significant improvements. Here’s how HOW.EDU.VN can assist you:
13.1 How to Schedule a Consultation
- Visit Our Website: Go to HOW.EDU.VN and navigate to the “Consultation” section.
- Fill Out the Form: Provide detailed information about your symptoms, medical history, and concerns.
- Select a Specialist: Choose an expert who specializes in your specific bladder health issue.
- Schedule Your Appointment: Select a date and time that works for you, and confirm your appointment.
13.2 What to Expect During Your Consultation
- In-Depth Assessment: Our specialist will conduct a thorough assessment of your symptoms and medical history.
- Diagnostic Recommendations: We will recommend appropriate diagnostic tests to identify the underlying causes of your bladder problems.
- Personalized Treatment Plan: We will develop a customized treatment plan tailored to your specific needs and goals.
- Ongoing Support: Our team will provide ongoing support and education to help you manage your bladder health effectively.
13.3 Success Stories from HOW.EDU.VN Clients
Many clients have experienced significant improvements in their bladder health after consulting with our experts at HOW.EDU.VN. These success stories highlight the effectiveness of personalized treatment plans and ongoing support.
14. Practical Tips for Daily Bladder Management
Implementing simple yet effective daily habits can significantly improve your bladder management and overall quality of life.
14.1 Establish a Regular Voiding Schedule
Establishing a regular voiding schedule can help train your bladder and reduce urgency. Try to urinate every 2-3 hours, even if you don’t feel the urge.
14.2 Practice Double Voiding
Double voiding involves urinating, waiting a few seconds, and then urinating again. This technique can help ensure complete bladder emptying and reduce the risk of urinary retention.
14.3 Stay Active and Maintain a Healthy Weight
Regular physical activity and maintaining a healthy weight can improve overall health and bladder function.
14.4 Monitor Your Fluid Intake
Monitor your fluid intake throughout the day and avoid drinking large amounts of fluids before bedtime.
15. Frequently Asked Questions (FAQs) About Bladder Capacity
To address common queries, here are some frequently asked questions about bladder capacity:
- What is the average bladder capacity for adults?
- The average bladder capacity for adults is between 300 to 500 ml (10 to 17 ounces).
- How can I increase my bladder capacity?
- Bladder training, pelvic floor exercises, and dietary adjustments can help improve bladder capacity.
- What are the symptoms of reduced bladder capacity?
- Symptoms include frequent urination, urgency, nocturia, and urinary incontinence.
- Can medical conditions affect bladder capacity?
- Yes, conditions such as overactive bladder, urinary tract infections, and interstitial cystitis can impact bladder capacity.
- How is bladder capacity diagnosed?
- Diagnosis involves medical history, physical exam, bladder diary, urinalysis, urodynamic testing, and cystoscopy.
- Are there medications to improve bladder capacity?
- Yes, medications such as anticholinergics can help reduce bladder spasms and urgency.
- What is the role of pelvic floor exercises in bladder control?
- Pelvic floor exercises strengthen the muscles that support the bladder, improving control and reducing leakage.
- How does diet affect bladder capacity?
- Certain foods and drinks can irritate the bladder, reducing its functional capacity.
- Can age affect bladder capacity?
- Yes, as people age, the bladder’s elasticity and capacity may decrease.
- When should I seek expert advice for bladder problems?
- If you experience persistent or severe bladder symptoms, consult with a healthcare professional for proper diagnosis and treatment.
Navigating the complexities of bladder capacity requires a comprehensive understanding and, often, expert guidance. At HOW.EDU.VN, we are committed to providing you with the knowledge and support you need to achieve optimal bladder health.
Don’t let bladder issues control your life. Contact our team of over 100 renowned PhDs at HOW.EDU.VN for personalized advice and effective solutions. Reach out to us today at 456 Expertise Plaza, Consult City, CA 90210, United States, or call us on WhatsApp at +1 (310) 555-1212. Visit our website at how.edu.vn to schedule your consultation and take the first step towards regaining control over your bladder health.