Insulin cost to make is surprisingly low, but the final insulin price often presents a significant financial burden for patients; HOW.EDU.VN connects you with leading experts to navigate the complexities of medication costs. We will explore factors driving insulin prices and strategies to find affordable options, ensuring you receive the treatments you need without financial strain. Discover expert insights on diabetes management and cost-effective solutions, including drug pricing dynamics, pharmaceutical economics, and potential cost-saving strategies.
1. What Is the Actual Cost to Manufacture Insulin?
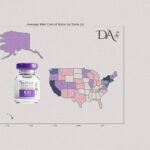
The actual cost to manufacture insulin is significantly lower than the price many patients pay. Estimates suggest that producing a vial of insulin costs between $2 to $4. This stark contrast between manufacturing costs and market prices raises questions about the factors contributing to the high cost of insulin for consumers.
1.1. Production Process and Cost Breakdown
The modern production of insulin involves advanced biotechnology. Here’s a breakdown of the typical process and associated costs:
- Genetic Engineering: Inserting the human insulin gene into bacterial DNA.
- Fermentation: Cultivating bacteria to produce insulin.
- Purification: Extracting and purifying insulin from the bacterial culture.
- Quality Control: Ensuring the insulin meets stringent quality standards.
- Packaging: Preparing insulin for distribution, including vials and cartridges.
1.2. Historical Context of Insulin Production
Initially, insulin was extracted from animal pancreases. However, modern methods using recombinant DNA technology have streamlined production, theoretically reducing costs. Despite these advancements, the price of insulin has continued to rise, outpacing inflation and technological improvements.
2. Why Is Insulin So Expensive Despite the Low Manufacturing Cost?
Several factors contribute to the high cost of insulin, despite the low manufacturing costs. These include market dynamics, regulatory issues, and the complex interplay between pharmaceutical companies, insurance providers, and pharmacy benefit managers.
2.1. Market Monopoly and Lack of Competition
The insulin market is dominated by three major manufacturers: Eli Lilly, Sanofi, and Novo Nordisk. This oligopoly allows these companies to control prices with minimal competitive pressure. The lack of biosimilar competition further exacerbates the issue.
- Eli Lilly: A leading global pharmaceutical company with a long history in insulin production.
- Sanofi: Another major player, offering a range of insulin products and diabetes solutions.
- Novo Nordisk: A key manufacturer focused on diabetes care, including insulin delivery systems.
2.2. The Role of Pharmacy Benefit Managers (PBMs)
Pharmacy Benefit Managers (PBMs) act as intermediaries between drug manufacturers and insurance companies. They negotiate drug prices, create formularies, and process prescription claims. However, their practices often lead to higher insulin prices.
2.2.1. Rebates and List Prices
PBMs negotiate rebates from drug manufacturers in exchange for placing their products on preferred drug lists. These rebates are often a percentage of the list price, incentivizing PBMs to favor drugs with higher list prices, as this increases their rebate revenue.
2.2.2. Impact on Patients
This system negatively affects patients, particularly those with high-deductible health plans or those who are uninsured. These individuals often pay the full list price of insulin, which can be significantly inflated due to the rebate system.
2.3. Regulatory and Patent Issues
Regulatory and patent issues also play a role in the high cost of insulin. Evergreening, a practice where pharmaceutical companies extend patent protection by making minor modifications to existing drugs, can delay the entry of biosimilars into the market.
2.3.1. Evergreening
Evergreening involves obtaining new patents for slightly modified versions of existing drugs. This extends market exclusivity and prevents competition from generic or biosimilar products, allowing manufacturers to maintain high prices.
2.3.2. Biosimilar Delays
The introduction of biosimilars—drugs that are highly similar to existing biologic drugs—can lower prices by increasing competition. However, regulatory hurdles and patent disputes often delay the availability of biosimilars in the U.S. market.
2.4. Lack of Price Regulation
Unlike many other countries, the United States does not have government regulations to control drug prices. This lack of regulation allows manufacturers to set prices at levels that maximize profits, contributing to the high cost of insulin.
3. What Are the Different Types of Insulin and Their Costs?
Insulin comes in various types, each with different onset times, durations, and costs. Understanding these differences can help patients and healthcare providers make informed decisions about insulin therapy.
3.1. Rapid-Acting Insulin
Rapid-acting insulin starts working within 15 minutes, peaks in about an hour, and lasts for 2-4 hours. It is often used before meals to cover carbohydrate intake.
- Examples: Lispro (Humalog), Aspart (NovoLog), Glulisine (Apidra)
- Typical Use: Mealtime insulin
3.2. Short-Acting Insulin
Short-acting insulin starts working within 30 minutes, peaks in 2-3 hours, and lasts for 3-6 hours. It is also used before meals but requires a longer waiting period.
- Examples: Regular (Humulin R, Novolin R)
- Typical Use: Mealtime insulin
3.3. Intermediate-Acting Insulin
Intermediate-acting insulin starts working in 2-4 hours, peaks in 4-12 hours, and lasts for 12-18 hours. It is often used to provide basal insulin coverage.
- Examples: NPH (Humulin N, Novolin N)
- Typical Use: Basal insulin
3.4. Long-Acting Insulin
Long-acting insulin starts working several hours after injection and provides a steady level of insulin for 24 hours or longer. It is used to provide basal insulin coverage.
- Examples: Glargine (Lantus, Basaglar), Detemir (Levemir), Degludec (Tresiba)
- Typical Use: Basal insulin
3.5. Pre-Mixed Insulin
Pre-mixed insulin combines different types of insulin in one vial or pen, providing both mealtime and basal coverage.
- Examples: Humulin 70/30, Novolin 70/30, NovoLog Mix 70/30
- Typical Use: Convenience for those needing both basal and mealtime insulin
3.6. Cost Comparison of Different Insulin Types
The cost of insulin can vary significantly depending on the type, brand, and formulation. Here is a general comparison:
| Insulin Type | Brand Examples | Average Cost per Vial | Notes |
|---|---|---|---|
| Rapid-Acting | Humalog, NovoLog, Apidra | $250 – $350 | Generally more expensive; often used with insulin pumps. |
| Short-Acting | Humulin R, Novolin R | $100 – $200 | Less expensive; requires careful timing with meals. |
| Intermediate-Acting | Humulin N, Novolin N | $100 – $200 | Provides basal coverage; can be less predictable than long-acting insulins. |
| Long-Acting | Lantus, Basaglar, Tresiba | $300 – $400 | Provides stable basal coverage; biosimilars like Basaglar can be more affordable. |
| Pre-Mixed | Humulin 70/30, NovoLog Mix | $150 – $250 | Convenient but less flexible; may not suit everyone’s needs. |
Note: Prices are estimates and can vary based on location, pharmacy, and insurance coverage.
4. What Are the Consequences of High Insulin Costs?
The high cost of insulin has severe consequences for individuals with diabetes, leading to financial strain, compromised health outcomes, and increased mortality.
4.1. Insulin Rationing
Faced with high costs, many patients resort to insulin rationing, which involves using less insulin than prescribed to stretch their supply. This can lead to serious health complications.
- Reduced Doses: Taking smaller doses than prescribed.
- Skipping Doses: Omitting doses altogether.
- Stretching Supply: Using expired insulin.
4.2. Health Complications
Insulin rationing can result in uncontrolled blood sugar levels, leading to:
- Diabetic Ketoacidosis (DKA): A life-threatening condition caused by a buildup of ketones in the blood.
- Hyperglycemia: High blood sugar levels, which can cause damage to organs and tissues over time.
- Long-Term Complications: Increased risk of heart disease, kidney failure, blindness, and amputations.
4.3. Increased Mortality
In severe cases, insulin rationing can be fatal. Several deaths have been reported among individuals who could not afford insulin and resorted to dangerous rationing practices.
5. What Strategies Can Individuals Use to Lower the Cost of Insulin?
Despite the challenges, several strategies can help individuals lower the cost of insulin and ensure they receive the treatment they need.
5.1. Patient Assistance Programs (PAPs)
Many pharmaceutical companies offer patient assistance programs to help eligible individuals access insulin at a reduced cost or for free.
- Eligibility Criteria: Typically based on income, insurance status, and medical need.
- Application Process: Requires filling out an application and providing documentation of income and medical information.
5.2. Generic and Biosimilar Options
Choosing generic or biosimilar insulin can significantly lower costs compared to brand-name products.
- Generics: Chemically identical to brand-name insulins and available for short-acting and intermediate-acting insulins.
- Biosimilars: Highly similar to brand-name biologic insulins and can offer substantial savings.
5.3. Discount Programs and Coupons
Various discount programs and coupons can help lower the cost of insulin.
- GoodRx: A website and app that provides coupons and discounts on prescription drugs.
- Manufacturer Coupons: Coupons offered directly by insulin manufacturers.
5.4. Switching to Less Expensive Insulin Types
Working with a healthcare provider to switch to a less expensive type of insulin can also help lower costs.
- NPH and Regular Insulin: Less expensive options for basal and mealtime insulin.
- Considerations: Requires careful monitoring and adjustment of dosages.
5.5. State and Federal Programs
Several state and federal programs offer assistance with prescription drug costs.
- Medicare Part D: Provides prescription drug coverage for Medicare beneficiaries.
- State Pharmaceutical Assistance Programs (SPAPs): Offer additional assistance to eligible residents.
5.6. Purchasing Insulin from Canada
Purchasing insulin from Canada can be a more affordable option for some individuals, as prices are typically lower than in the U.S.
- Requirements: Requires a prescription from a U.S. healthcare provider.
- Considerations: Ensure the pharmacy is reputable and the insulin is properly stored and transported.
6. What Policy Changes Are Needed to Address the Insulin Pricing Crisis?
Addressing the insulin pricing crisis requires comprehensive policy changes to increase competition, regulate prices, and ensure affordable access to this life-saving medication.
6.1. Price Regulation
Implementing price regulation can prevent manufacturers from setting exorbitant prices for insulin.
- Government Negotiation: Allowing the government to negotiate drug prices with manufacturers.
- Price Caps: Setting limits on how much manufacturers can charge for insulin.
6.2. Increased Competition
Encouraging competition through the expedited approval of biosimilars can help lower prices.
- Streamlined Approval Process: Simplifying the regulatory process for biosimilars.
- Incentives for Manufacturers: Providing incentives for manufacturers to develop and market biosimilars.
6.3. Transparency in Pricing
Requiring transparency in pricing can help expose the markups and rebates that contribute to the high cost of insulin.
- Disclosure Requirements: Mandating that manufacturers, PBMs, and insurers disclose pricing information.
- Public Reporting: Making pricing data publicly available to increase accountability.
6.4. Capping Out-of-Pocket Costs
Capping out-of-pocket costs for insulin can protect patients from financial hardship.
- Co-Pay Limits: Setting limits on how much patients pay for insulin each month.
- Subsidy Programs: Providing subsidies to help low-income individuals afford insulin.
6.5. Legislative Efforts
Legislative efforts at both the state and federal levels are needed to address the insulin pricing crisis.
- The Inflation Reduction Act: Caps insulin co-payments for Medicare beneficiaries at $35 a month.
- State Laws: Some states have enacted laws to cap insulin prices or provide emergency access to insulin.
7. How Can Healthcare Providers Help Patients Manage Insulin Costs?
Healthcare providers play a crucial role in helping patients manage insulin costs by providing information, support, and guidance on affordable options.
7.1. Discussing Cost Concerns
Openly discussing cost concerns with patients can help healthcare providers identify financial barriers to insulin access.
- Routine Screening: Incorporating cost-of-care discussions into routine appointments.
- Empathy and Support: Providing a supportive environment for patients to share their concerns.
7.2. Prescribing Affordable Options
Healthcare providers can prescribe more affordable insulin options, such as generics or biosimilars, when appropriate.
- Clinical Considerations: Ensuring the chosen insulin is safe and effective for the patient.
- Patient Education: Educating patients about the benefits and risks of different insulin types.
7.3. Connecting Patients with Resources
Healthcare providers can connect patients with resources that can help them lower the cost of insulin, such as patient assistance programs, discount programs, and state and federal programs.
- Referral Networks: Establishing referral networks with local organizations that provide financial assistance.
- Information Sharing: Providing patients with up-to-date information on available resources.
7.4. Monitoring and Follow-Up
Regular monitoring and follow-up can help ensure patients are able to afford and adhere to their insulin regimen.
- Blood Sugar Monitoring: Tracking blood sugar levels to assess the effectiveness of treatment.
- Adherence Support: Providing support and encouragement to help patients adhere to their insulin regimen.
8. What Is the Future of Insulin Pricing and Accessibility?
The future of insulin pricing and accessibility depends on the collective efforts of policymakers, manufacturers, healthcare providers, and patient advocates to address the systemic issues that contribute to the high cost of this life-saving medication.
8.1. Technological Advancements
Technological advancements in insulin delivery and monitoring may help lower costs and improve outcomes.
- Insulin Pumps: Advanced insulin pumps can deliver precise doses of insulin and reduce waste.
- Continuous Glucose Monitors (CGMs): CGMs can provide real-time blood sugar readings and help patients adjust their insulin doses accordingly.
8.2. Advocacy and Awareness
Continued advocacy and awareness are essential to keep the pressure on policymakers and manufacturers to address the insulin pricing crisis.
- Patient Advocacy Groups: Organizations like T1International are working to raise awareness and advocate for policy changes.
- Public Education Campaigns: Educating the public about the high cost of insulin and its impact on individuals with diabetes.
8.3. Collaborative Solutions
Collaborative solutions involving all stakeholders are needed to create a sustainable and equitable system for insulin pricing and accessibility.
- Dialogue and Negotiation: Encouraging dialogue and negotiation between manufacturers, PBMs, insurers, and patient advocates.
- Shared Responsibility: Recognizing that all stakeholders have a role to play in ensuring affordable access to insulin.
9. Expert Insights on Managing Diabetes and Insulin Costs
Navigating diabetes management and insulin costs can be overwhelming. Here are some expert insights to help you stay informed and proactive.
9.1. Kasia Lipska, MD, MHS
Associate Professor of Medicine (Endocrinology) at Yale School of Medicine, Dr. Lipska has conducted extensive research on insulin affordability and rationing. Her work highlights the widespread impact of high insulin costs and the urgent need for policy changes.
9.2. Additional Resources
- American Diabetes Association (ADA): Offers resources and support for individuals with diabetes.
- JDRF (Juvenile Diabetes Research Foundation): Funds research and advocates for people with type 1 diabetes.
- T1International: A patient-led organization advocating for affordable insulin access.
10. How Can HOW.EDU.VN Help?
At HOW.EDU.VN, we understand the challenges individuals face in navigating the complexities of insulin costs and diabetes management. Our platform connects you with leading experts who can provide personalized guidance and support.
10.1. Access to Top Experts
We offer access to a network of over 100 world-renowned Ph.Ds who specialize in endocrinology, pharmaceutical economics, and healthcare policy. These experts can provide insights into:
- Cost-effective diabetes management strategies
- Understanding drug pricing dynamics
- Navigating insurance and patient assistance programs
10.2. Personalized Consultations
Our Ph.Ds offer personalized consultations tailored to your specific needs. Whether you are seeking advice on finding affordable insulin options, understanding your insurance coverage, or advocating for policy changes, our experts can provide the guidance you need.
10.3. Comprehensive Support
We provide comprehensive support to help you manage your diabetes and reduce your insulin costs. This includes:
- Educational resources on insulin types and costs
- Information on patient assistance programs and discount options
- Guidance on working with your healthcare provider to optimize your treatment plan
10.4. Addressing Your Challenges
We recognize the challenges our clients face in accessing affordable healthcare. Whether it’s the difficulty in finding qualified experts, the high cost of consultations, or concerns about the reliability of information, HOW.EDU.VN is committed to providing solutions that are:
- Accessible: Connect directly with top experts from around the world.
- Affordable: Save time and money with expert guidance tailored to your needs.
- Reliable: Ensure the confidentiality and trustworthiness of your consultations.
The cost to make insulin remains a fraction of what many patients pay, highlighting systemic issues in pricing and accessibility. By understanding these issues and exploring available strategies, individuals can take proactive steps to manage their insulin costs and ensure they receive the care they need. For expert guidance and personalized support, contact HOW.EDU.VN today. Let our team of over 100 world-renowned Ph.Ds assist you in navigating the complexities of diabetes management and securing affordable insulin solutions.
Are you struggling with high insulin costs and need expert advice? Contact HOW.EDU.VN today for personalized guidance from our team of over 100 world-renowned Ph.Ds. We can help you navigate the complexities of diabetes management, understand your insurance options, and find affordable insulin solutions. Don’t let financial barriers compromise your health. Reach out to us at 456 Expertise Plaza, Consult City, CA 90210, United States, Whatsapp: +1 (310) 555-1212, or visit our website at how.edu.vn. Your health and well-being are our top priorities.
FAQ: Frequently Asked Questions About Insulin Costs
1. What Is the Average Cost of Insulin per Month?
The average monthly cost of insulin can vary widely, ranging from $300 to $600 or more, depending on the type of insulin, dosage, and insurance coverage.
2. Why Has the Price of Insulin Increased So Much?
The price of insulin has increased due to factors such as market monopolies, lack of competition, the role of pharmacy benefit managers, regulatory issues, and lack of price regulation.
3. What Are Biosimilars and Can They Lower Insulin Costs?
Biosimilars are drugs that are highly similar to existing biologic drugs. They can offer substantial savings by increasing competition in the market.
4. How Can I Find Patient Assistance Programs for Insulin?
You can find patient assistance programs by contacting the insulin manufacturers directly or visiting their websites. Resources like the American Diabetes Association can also provide information.
5. Is It Safe to Purchase Insulin from Canada?
Purchasing insulin from Canada can be a more affordable option, but it’s important to ensure the pharmacy is reputable and the insulin is properly stored and transported. Always consult with your healthcare provider.
6. What Should I Do If I Can’t Afford My Insulin?
If you can’t afford your insulin, talk to your healthcare provider about switching to a less expensive type of insulin, explore patient assistance programs, and check for discount coupons.
7. What Is Insulin Rationing and Why Is It Dangerous?
Insulin rationing is using less insulin than prescribed to stretch your supply. It is dangerous because it can lead to uncontrolled blood sugar levels and serious health complications.
8. How Does the Inflation Reduction Act Affect Insulin Costs?
The Inflation Reduction Act caps insulin co-payments for Medicare beneficiaries at $35 a month, providing relief for many seniors.
9. Can My Healthcare Provider Help Me Lower My Insulin Costs?
Yes, your healthcare provider can help you by prescribing affordable options, connecting you with resources, and discussing cost concerns openly.
10. What Policy Changes Are Needed to Make Insulin More Affordable?
Policy changes needed include price regulation, increased competition, transparency in pricing, capping out-of-pocket costs, and legislative efforts at the state and federal levels.